Pathology of complications of COM
Routes of spread of infection:
Whether acute or chronic, the infection from the middle ear spreads via:
1. Extension through bone that has been demineralised during acute infections, or resorbed by cholesteatoma, or osteitis in chronic disease of the ear. Demineralisation is brought about by various enzymes that are released during the acute infections. Cholesteatoma causes bone erosion either due to pressure necrosis, or halisterisis. Halisterisis is also known as hyperimic decalcification. As the term itself suggests decalcification is caused by hyperaemia.
2. Spread through venous channels: Spreading of infected clot within small veins through the bone and dura into the dural venous sinuses. If spread via this route occurs then the infection may find its way into the brain without involving the bone or dura. Thrombophlebitis from the lateral sinus may spread to the cerebellum, and from the superior petrosal sinus may spread to the temproral lobe of the brain.
3. Spread through normal anatomical pathways: Spread may occur through oval / round windows into the internal auditory meatus. Spread may also occur through the cochlear and vestibular aqueducts. Certain areas may have dehiscent bone as a normal variant i.e. bony covering of the jugular bulb, dehiscent areas in the tegmen tympani, and dehiscent suture lines of the temporal bone.
4. Spread may occur through non anatomical bony defects like those caused due to trauma, (accident, surgical) or by erosion due to neoplasia.
5. Spread may occur through surgical defects as caused by fenestration of the oval window during stapedectomy procedures.
6. Spread may occur directly into the brain tissue through the peri arteriolar spaces of Virchow Robin. This spread does not affect the cortical arterioles perse, hence abscess occur in the white matter without the involvement of gray matter of brain.
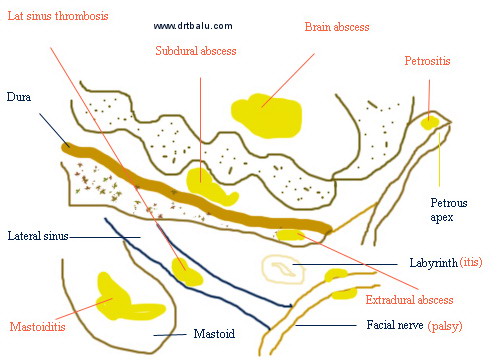
Diagram showing various intracranial complications
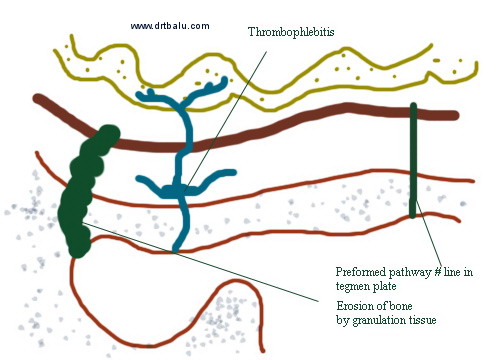
Diagram illustrating route of spread of middle ear infection
Prevalence rates for compliations of COM (both extracranial & intracranial) ranges between 0.6-5%. The most common extracranial complication happens to be mastoid abscess also known as subperiosteal abscess. Cholesteatoma has been implicated with major complications intracranially.
Labyrinthine fistula:
This is one of the complication of active mucosal COM / cholesteatoma. This can cause severe sensorineural hearing loss by affecting the cochlear membranes including the hair cells. Suppression of inflammatory mediators by using steroids before administration of antibiotics could help these patients.
Histologically cholesteatoma matrix / granulation tissue could become apposed to the endosteum of the inner ear mediating inflammatory reaction in the inner ear fluid. In many fistulae reactive inner ear changes could be absent because of protective walling off of the inflammatory mediators. In addition the margins of the labyrinthine fistulae could should evidence of new bone formation which could eventually close the opening.
Labyrinthitis:
- This is defined as an inflammatory disorder involving the inner ear / labyrinth. Clinically this condition causes disturbances of balance and hearing of varying degrees in the involved ear.
- Causes:
- 1. Bacterial infections
- 2. Viral infections
- 3. Autoimmune causes
- 4. Vascular ischemic causes
- Pathophysiology:
- Anatomically labyrinth is composed of an outer osseous framework surrounding the delicate membranous labyrinth which contains the peripheral end organs of hearing and balance. Membranous labyrinth include:
- 1. Utricle
- 2. Saccule
- 3. Semicircular canals
- 4. Cochlea
The labyrinth lies within the petrous portion of temporal bone. It communicates with the middle ear via the oval and round windows.
Infecting organism may find their way into the inner ear via:
- Pre-existing fractures
- Oval window
- Round window
- Congenital dehiscence involving the bony labyrinth
- Viral labyrinthitis: Is characterized by sudden unilateral loss of hearing and equilibrium. Vertigo is usually incapacitating and associated with vomiting. These patients are bed ridden. Vertigo usually subsides within 4-6 weeks. Hearing loss is confined to high frequencies and is sensorineural in nature. An attack of upper respiratory tract infection precedes the development of labyrinthitis. This condition should not be compared with vestibular neuronitis which involves only the vestibular nerves and spares the cochlear component. Varicella Zoster oticus is an unique form of viral labyrinthitis caused by reactivation of dormant varicella zoster virus. This reactivated virus is known to attack spiral ganglion.
- Common viral causes of labyrinthitis:
- 1. Mumps
- 2. Measles
- 3. Rubella (congenital labyrinthitis)
4. Cytomegalovirus
Bacterial labyrinthitis: can be potentially caused by meningitis / otitis media. This could be caused by direct invasion of membranous labyrinth by the infecting organism (suppurative labyrinthitis) causing permanent destruction of vestibular and cochlear end organs. In patients with meningitis spread of infections can be bilateral since infections can travel via the CSF and involve the inner ear fluids through the internal acoustic meatus / cochlear aqueduct. Bacterial infections involving the middle ear cavity can enter the labyrinth via erosion of lateral canal which is commonly seen in patients with cholesteatoma. Treatment is usually directed against infecting organism and supportive therapy. Suppurative labyrinthitis is usually followed by labyrinthitis ossificans where the whole of the membranous labyrinth gets ossified. Labyrinthitis ossificans indicates a permanently dead labyrinth.
Common bacterial causes of labyrinthitis include:
-
- S. pnuemoniae
- Haemophilus influenza
- Streptococcus
- Staphylococcus
- Neisseria
- Bacteroids
- Proteus
- Moraxella catarrhalis
- Serous labyrinthitis:
This is a potentially reversible disorder caused by diffusion of bacterial toxins into the inner ear via the inflamed round window membrane. Studies have shown that the permeability of the round window membrane is increased when there is inflammation. This may cause diffusion of bacterial toxins and immune mediators into the inner ear causing transient impairment of the inner ear functions.
Facial nerve paralysis:
The frequency of facial paralysis ranges between 0.5-2.5%. Granulation tissue / cholesteatoma may cause facial nerve paralysis when dehiscence of this nerve is present / the bony covering is eroded by cholesteatoma matrix. Prognosis of facial nerve paralysis is worse when it is caused by COM than Bell's palsy.
Hearing loss:
COM can produce inflammatory changes in the round window area causing inflammation to spread to membranous portion of the cochlea. There is loss of both inner and outer hair cells leading on to sensorineural hearing loss.
