Chronic otitis media
E mail
Chronic otitis media is defined as chronic infection of mucosa lining the middle ear cleft and mastoid cavity. Middle ear cleft includes the middle ear proper and the eustachean tube. Diagnosis of Chronic otitis media implies a permanent abnormality of pars tensa / pars flaccida portion of the ear drum.
This condition most likely is a result of:
1. Earler episodes of acute otitis media
2. Negative middle ear pressure
3. Otitis media with effusion
It should be stressed that chronic inflammation of middle ear cavity is not necessarily associated with a perforated ear drum.
Complications of COM is mostly due to inflammation extending outside the confines of the middle ear cleft.
The following features are some of the evidence of reparative process:
Vascular granulation tissue
New bone formation
Use of microscope is performing routine otological examination is common these days. It allows both hands of the surgeon free to clean the external canal, suck out the secretions and to examine the ear drum under magnification. This has also done away the concept of tubotympanic and atticoantral disease. The tern safe and unsafe ear is also not used these days.
Initially tubotympanic middle ear disease which involves middle ear cleft alone is considered to be a safe disease as dangerous complications were not common where as attico antral disease that involves the attic region of the middle ear cavity is considered tobe a dangerous variety of otitis media because rates of complications were found tobe a bit high.
High incidence of complications in atticoantral disease is due to:
1. The proximity of the area to skull base
2. Crowding of structures seen in this area
But current understanding of pathophysiology of chronic otitis media after the advent of routine microscopic examination of the ear has undergone lots of changes that has been incorporated into the currently acceptable classification of chronic otitis media types.
Active COM:
In this condition there is inflammation of middle ear mucosa associated with accumulation of pus. There may also be associated mastoiditis. Active COM can be subdivided into active mucosal COM and active squamosal COM.
Active mucosal COM:
Ear drum in these patients will be perforated. The middle ear mucosa may undergo polypoidal changes causing "aural polypi". It is also important to realize that inflammatory changes in this disorder is not confined to the middle ear alone, the whole of the middle ear cleft is involved. Simple closure of the perforation without removal of infected middle ear mucosa and granulations from the mastoid cavity is fraught with failure to control the disease.
Active mucosal COM is often associated with resorption of parts or whole of ossicular chain. This could be due to resorptive osteitis. The ossicles affected typically show hyperemia with proliferation of capillaries and prominent histiocytes. Long process of incus gets eroded commonly, followed by stapes crurae, body of incus and manubrium in that order.
Active squamous COM:
This condition is otherwise known as unsafe ear or cholesteatoma. This condition is commonly associated with retraction of pars flaccida / tensa that has retained squamous epithelial debris. There is also associated inflammation of middle ear mucosa, production of pus, and erosion of ossicles. This condition is commonly associated with intracranial complications.
Inactive Chronic otitis media:
In this condition the middle ear mucosa is relatively healthy. The mastoid cavity also appear healthy. These patients may slip into active phase rather easily because of the existing pathology. Inactive chronic otitis media can further be subdivided into Inactive mucosal chronic otitis media and Active squamous chronic otitis media.
Inactive mucosal chronic otitis media:
This condition is always associated with dry perforation of the ear drum. There is permanent perforation of the pars tensa, but the middle ear and mastoid mucosa are not inflamed. The drum remnant around the perforation is always healthy. The rim of the perforation is thickened due to proliferation of fibrous tissue. Squamous epithelial cells from the external auditory canal does not migrate into the middle ear cavity in this stage because the annulus of the ear drum is intact and it prevents this migration. These patients benefit from myringoplasty.
Inactive squamous epithelial chronic otitis media:
These include retraction pockets, atelectasis and epidermization. Negative middle ear pressure can cause retraction of tympanic membrane. A retraction pocket consists of an invagination into the middle ear space of part of the ear drum. These retraction pockets may be fixed when it is adherent to structures in the middle ear or free when it can move freely medially or laterally depending on the state of inflation of the middle ear. "Epidermization" is a more advanced type of retraction and it refers to replacement of middle ear mucosa by keratinizing squamous epithelium without retention of keratin debris. The area of epidermization may involve part or all of the middle ear cavity. Epidermization often remain quiescent and does not progress to cholesteatoma or active suppuration. So epidermization per se is not an indication for surgical intervention.
Healed chronic otitis media:
In this stage the perforated ear drum has managed to heal itself. Loss of lamina propria or the tympanic membrane due to atrophy or failure of complete healing leads to a 'dimeric' membrane that consists of epidermis and mucosa only. Such thin membrane is more prone to retraction if there is negative middle ear pressure.
Tympanoslcerosis is also another form of healed ear drum. It refers to hyaline deposits of acellular material visible as whitish plaques in the tympanic membrane or as white nodular deposits in the submucosal layers of the middle ear on otoscopy. Tympanosclerosis is the end result of a healing process in which collagen in fibrous tissue hyalinizes, loses its structure and become fused into a homogenous mass. Calcification and ossification may occur to a variable extent.
It is an accepted fact that chronic otitis media commonly starts with episodes of acute otitis media (AOM) or otitis media with effusion (OME) in childhood. OME leads to thinning of ear drum, hearing loss and delayed speech development.
COM can be characterized histopathologically by middle ear pathology like granulation tissue, cholesterol granuloma or cholesteatoma formation.
Active COM is chronic inflammation of middle ear / mastoid mucosa with recurrent discharge of atleast 2 weeks through chronic perforation of the ear drum.
Otitis media and chronic otitis media are multifactorial diseases involving no single genetic defect making it impossible to identify the single offending gene. Patient factors also play an important role in pathogenesis of COM. These factors include:
1. Innate immunity of the patient to the disease (toll-like receptors, cytokines and surfactants). Toll like receptors are pattern recognition receptors that are involved in the innate immune system against microbes. Toll like receptor 4 responds to and recognizes the lipopolysaccharide of gram negative bacteria. The innate immune system is the first line of defence against gram negative infections of middle ear cavity.
2. Adaptive immunity of the patient (Immunoglobulins)
3. Non specific immunity (presence of epithelial barriers and mucin production)
4. Inflammation regulation
5. Craniofacial abnormalities
Otitis media is cuaed by bacteria entering via the Eustachean tube. At this point it should be stressed that sterile otitis media is not that uncommon and initiation of inflammation in this scenario is rather unclear.
Various genetic models used to study pathogenesis of COM demonstrated hypoxia and hypoxia inducible factor (HIF) could be the mechanism involved in chronic inflammatory process of middle ear mucosa. HIF signalling is regulated at the transcriptional level by interactions with the master regulator of inflammation Nuclear factor kappa-light-chain-enhancer of activated B cells. At the translational level it is regulated by cytokines which are glycoproteins produced by inflammatory cells and epithelial cells like interleukin-1 amd TNF alpha.
Nuclear factor kappa-light-chain-enhancer can be activated by many factors they include:
Cytokines
Bacterkal lipopolysaccharides
Viral pathogens
Growth factors
Vascular endothelial growth factor also has been postulated to play a role in OME. Hypoxia drives inflammation by activation of Nuclear factor kappa-light-chain-enhancer, Interleukin-1 beta and Tumor necrosis factor-alpha increases angiogenisis, vascular permeability and recruitment of neutrophils through activation of vascular endothelial growth factor. Introduction of tymponostomy tubes (grommet) improves oxygenation of middle ear cavity downgrading IHF signalling.
Recruitment of inflammatory cells (neutrophils, mast cells, lymphocytes, plasma cells or monocytes/macrophages are integral to the initiation of chronic inflammation of middle ear mucosa. Once the inflammation has been initiated, there is accumulation of fluid and inflammatory cells in the middle ear cavity causing conductive deafness and rarely sensorineural hearing loss due to diffusion of cytokines through the round window membrane. Permeability of round window membrane is increased during the inflammatory process.
TNF-alpha and Interleukin-8 increase inducible nitric oxide synthase in the middle ear mucosa. Nitric oxide stimulates mucin production.
This is actually a recent introduction. This condition is known to cause intractable middle ear pathology. This condition is characterised by excessive accumulation of eosinophils in the middle ear cavity and is associated with persistent middle ear effusion. In addition to this these patients also suffer from bronchial asthma. This condition is known to occur in patients with bronchial asthma who have T-helper type 2 dominant predisposition and also a patulous eustachean tube which allows entry of antigenic material into the middle ear cavity.
This condition was first described by Koch who reported some patients with middle ear effusion contained a large number of eosniophils. He also observed that middle ear secretions tended to be highly viscous and the middle ear mucosa appeared pinikish. This term was coined by Tomioka in 1993.
Pathophysiology:
Pathophysiology of this condition is obviously allergy. These patients commonly had associated allergic rhinitis and branchial asthma. Eosinophils could have been probably attracted to the middle ear cavity by the presence of IL 5 inside the middle ear cavity.
Features of Eosinophilic otitis media :
Sudden deterioration of hearing
Bronchial asthma
Allergic rhinitis
Intractable otitis media
Persistent otorrhoea
Incidence:
Incidence of eosinophlic otitis media is not clearly known. Literature search puts it to be rather common cause of otitis media with effusion.
Managment:
Patients diagnosed with this condition should be warned of the possibility of sudden deterioration of hearing.
Administration of systemic / topical steroids could be of benefit in these patients.
Antihistamines and leukotreine receptor antogonists can also be used with benefit.
Grommet insertion is indicated in patients with acute sudden hearing loss.
Inactive mucosal COM:
This condition involves dry cental perforation of pars tensa. In these patients there is permanent perforation of pars tensa. Middle ear mucosa and mucosal lining the mastoid cavity are not inflammed. The mucocutaneous junction is usually located at the margin of the perforation can extend up to the fibrous annulus.
Active mucosal COM (Perforation with otorrhoea):
In this category there is chronic inflammation of mucosa of the middle ear cavity and mastoid. Mucosa of middle ear cleft show varying degrees of oedema, submucosal fibrosis, hypervascularity and presence of inflammatory infiltrate that include lymphocytes, plasma cells and histiocytes. There is also associated increase in the number of goblet cells. Basal cell layer of middle ear mucosa also shows evidence of hyperplasia. Granulation tissue can occur and is described as aural polyp. It protrudes through the perforated ear drum.
In some areas with active COM (in both mucosal and cholesteatomatous subtypes) demonstrate focal areas of cholesterol granuloma formation. Cholesterol granuloma microscopically consists of a giant cell reaction surrounding cholesterol clefts.
Chronic inflammation is known to affect the entire middle ear cleft which include middle ear cavity proper, eustachean tube, aditus and antrum. During surgery granulation tissue from middle ear cavity, aditus, and antrum should be cleared. Active mucosal COM can cause destruction of ossicles of middle ear cavity. Ossicles show areas of hyperemia, proliferation of capillaries and formation of granulation tissue. Long process of incus commonly gets eroded because of its precarious blood supply, next to get affected would be the crura of stapes. Bacteria may also play a role in ossicular destruction especially in patients with cholesteatoma. Pseudomonas aeruginosa are known to cause destruction of ossicles by stimulating the inflammatory process.
Inactive squamous epithelial COM (Retraction, atelectasis and epidermization):
In this category of COM there is negative static middle ear pressure which is followed by retraction of ear drum (atelectasis). This retraction pocket consists of invaginated ear drum into the middle ear cavity. In fact a portion of this invagination could also be adherent to the structures of middle ear. If free of middle ear structural attachement ear drum moves freely on pneumatic otoscopy, if attached the mobility of ear drum could be restricted or absent.
Epidermization is advanced stage of this retraction process and it causes replacement of entire middle ear mucosa by keratinizing squamous epithelium, but without retention of keratin debris.
Active squamosal COM (Acquired cholesteatoma):
Cholesteatoma is defined as a cystic bag like structure lined by stratified squamous epithelium on a fibrous matrix. This sac contains desquamated squamous epithelium. This sac is present in the attic region. Cholesteatoma is also defined as 'skin in wrong place'. Cholesteatoma is known to contain all the layers of skin epithelium. The basal layer (germinating layer) is present on the outer surface of cholesteatoma sac in contact with the walls of the middle ear cleft. (This ofcourse is a old definition). This does not take into account the existence of pars tensa cholesteatoma where there is no retraction pocket as seen in pars flaccida cholesteatoma.
Cholesteatoma can cause destruction of local structures like ossicular chain, otic capsule leading on to complications like hearing loss, vestibular dysfunction, facial paralysis and intracranial disease / infection. The term cholesteatoma was first coined by the German Physiologist Johannes Muller in 1838.
Pathogenesis of cholesteatoma is due to retraction of pars flaccid or the posterior superior quadrant of pars tensa or retraction of entire pars tensa.
Theories of Active squamosal COM:
Cholesteatoma can also be classified according to its topology:
Attic cholesteatoma - This is actually a mixture of retraction pocket and papillary proliferation from the basal cell layer of squamous epithelium of pars flaccida.
Sinus cholesteatoma - This is a posteriosuperior retraction / perforation of pars tensa extending into the sinus tympani, posterior tympanum and beyond.
Tensa cholesteatoma - This is retraction and adhesion of the entire pars tensa and could involve tympanic orifice of eustachean tube.
Proliferation rate of cholesteatoma in comparison with that of skin lining of external canal is found to be 2.5 times higher. Defects in regulation of epidermal growth factor receptor system have also been identified in these patients. Current studies reveal that cholesteatoma arises from ear drum and not from skin lining of external canal / attic mucosa. This could account for the presence of cholesteatoma behind intact ear drum which has been classified under congenital cholesteatoma. Current literature does not acknowledge this condition as it is not a true congential disorder and does not fulfil the criteria for congenital disorders.
Congenital cholesteatoma:
Even though this condition is currently not accepted this is included for the sake of completeness of the topic.
This condition is known to arise from embryonic cell rests present in the middle ear cavity and temporal bone. These cell rests are known to commonly occur in cerebello pontine angle and petrous apex. Infact congenital cholesteatoma is seen as a whitish mass behind an intact tympanic membrane.
Derlacki and Clemis laid down the following as criteria to diagnose congenital cholesteatoma:
1. The patient should not have previous episodes of middle ear disease
2. Ear drum must be intact and normal
3. It is purely an incidental finding
4. If discharge and ear drum perforation is present then it should be contrued that congential cholesteatoma has managed to erode the tympanic membrane.
Clinical features: The disorder is an incidental finding. The common location of congenital cholesteatoma is the antero superior quadrant of tympanic membrane, postero superior quadrant being the next common site of involvement. Anteriorly situated congenital cholesteatomas are known to affect the eustachean tube function causing conductive deafness due to middle ear effusion, where as posterior congenital cholesteatoma is known to cause conductive deafness due to impairment of ossicular chain mobility.
Staging of congenital cholesteatoma:
Staging as suggested by Derlacki and Clemis: They were the first to stage congenital cholesteatoma. They classified congenital cholesteatoma into
1. Petrous pyramid cholesteatoma
2. Cholesteatoma involving the mastoid cavity
3. Cholesteatoma involving the middle ear cavity.
Potsic suggested the following staging mechanism:
Stage I : Single quadrant involvement with no ossicular / mastoid involvement.
Stage II : Multiple quadrant involvement with no ossicular / mastoid involvement
Stage III : Ossicular involvement without mastoid involvement
Stage IV : Mastoid extension
Nelson's staging:
Type I : Involvement of mesotympanum without involvement of incus / stapes
Type II : Involvement of mesotympanum / attic along with erosion of ossicles without extension into the mastoid cavity
Type III : Involvement of mesotympanum with mastoid extension
Staging this disease will help in deciding the modality of treatment and in predicting the long term prognosis.
Healed COM:
Nearly a quarter of patients with COM can undergo spontaneous healing. These patients show circular atrophy of ear drum indicating healed perforation. The presence of circular atrophy of ear drum could predispose it for reperforation due to further episodes of AOM / barotrauma. Other abnormalities found in the ear drum that could indicate healed com include tympanosclerosis.
Tympanosclerosis:
Is deposition of acellular hyaline and calcium deposits within the submucous layer of the tympanic membrane / submucous membrane of the middle ear cavity. In a majority of patients these plaques are so insignificant that they cause very little impairment in the hearing ability of the patient. These plaques could be likened to healed scar tissue.
When present over the tympanic membrane these plaques appear like a whitish cresentic shaped plaques.
Causes:
1. Could be caused by resolved otitis media.
2. Trauma
3. Chronic otitis media with effusion
4. After recurrent bouts of acute otitis media (middle ear tympanosclerosis)
5. After grommet insertion
6. Eustachean tube obstruction
Routes of spread of infection:
Whether acute or chronic, the infection from the middle ear spreads via:
1. Extension through bone that has been demineralised during acute infections, or resorbed by cholesteatoma, or osteitis in chronic disease of the ear. Demineralisation is brought about by various enzymes that are released during the acute infections. Cholesteatoma causes bone erosion either due to pressure necrosis, or halisterisis. Halisterisis is also known as hyperimic decalcification. As the term itself suggests decalcification is caused by hyperaemia.
2. Spread through venous channels: Spreading of infected clot within small veins through the bone and dura into the dural venous sinuses. If spread via this route occurs then the infection may find its way into the brain without involving the bone or dura. Thrombophlebitis from the lateral sinus may spread to the cerebellum, and from the superior petrosal sinus may spread to the temproral lobe of the brain.
3. Spread through normal anatomical pathways: Spread may occur through oval / round windows into the internal auditory meatus. Spread may also occur through the cochlear and vestibular aqueducts. Certain areas may have dehiscent bone as a normal variant i.e. bony covering of the jugular bulb, dehiscent areas in the tegmen tympani, and dehiscent suture lines of the temporal bone.
4. Spread may occur through non anatomical bony defects like those caused due to trauma, (accident, surgical) or by erosion due to neoplasia.
5. Spread may occur through surgical defects as caused by fenestration of the oval window during stapedectomy procedures.
6. Spread may occur directly into the brain tissue through the peri arteriolar spaces of Virchow Robin. This spread does not affect the cortical arterioles perse, hence abscess occur in the white matter without the involvement of gray matter of brain.
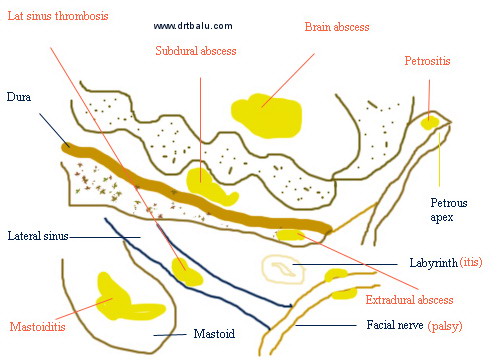
Diagram showing various intracranial complications
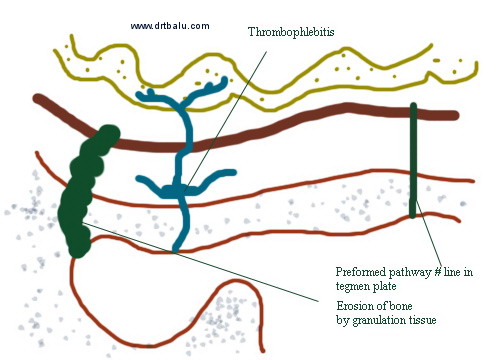
Diagram illustrating route of spread of middle ear infection
Prevalence rates for compliations of COM (both extracranial & intracranial) ranges between 0.6-5%. The most common extracranial complication happens to be mastoid abscess also known as subperiosteal abscess. Cholesteatoma has been implicated with major complications intracranially.
Labyrinthine fistula:
This is one of the complication of active mucosal COM / cholesteatoma. This can cause severe sensorineural hearing loss by affecting the cochlear membranes including the hair cells. Suppression of inflammatory mediators by using steroids before administration of antibiotics could help these patients.
Histologically cholesteatoma matrix / granulation tissue could become apposed to the endosteum of the inner ear mediating inflammatory reaction in the inner ear fluid. In many fistulae reactive inner ear changes could be absent because of protective walling off of the inflammatory mediators. In addition the margins of the labyrinthine fistulae could should evidence of new bone formation which could eventually close the opening.
Labyrinthitis:
The labyrinth lies within the petrous portion of temporal bone. It communicates with the middle ear via the oval and round windows.
Infecting organism may find their way into the inner ear via:
4. Cytomegalovirus
Bacterial labyrinthitis: can be potentially caused by meningitis / otitis media. This could be caused by direct invasion of membranous labyrinth by the infecting organism (suppurative labyrinthitis) causing permanent destruction of vestibular and cochlear end organs. In patients with meningitis spread of infections can be bilateral since infections can travel via the CSF and involve the inner ear fluids through the internal acoustic meatus / cochlear aqueduct. Bacterial infections involving the middle ear cavity can enter the labyrinth via erosion of lateral canal which is commonly seen in patients with cholesteatoma. Treatment is usually directed against infecting organism and supportive therapy. Suppurative labyrinthitis is usually followed by labyrinthitis ossificans where the whole of the membranous labyrinth gets ossified. Labyrinthitis ossificans indicates a permanently dead labyrinth.
Common bacterial causes of labyrinthitis include:
This is a potentially reversible disorder caused by diffusion of bacterial toxins into the inner ear via the inflamed round window membrane. Studies have shown that the permeability of the round window membrane is increased when there is inflammation. This may cause diffusion of bacterial toxins and immune mediators into the inner ear causing transient impairment of the inner ear functions.
Facial nerve paralysis:
The frequency of facial paralysis ranges between 0.5-2.5%. Granulation tissue / cholesteatoma may cause facial nerve paralysis when dehiscence of this nerve is present / the bony covering is eroded by cholesteatoma matrix. Prognosis of facial nerve paralysis is worse when it is caused by COM than Bell's palsy.
Hearing loss:
COM can produce inflammatory changes in the round window area causing inflammation to spread to membranous portion of the cochlea. There is loss of both inner and outer hair cells leading on to sensorineural hearing loss.
Acute otitis media and otitis media with effusion:
Acute otitis media and otitis media with effusion can cause long term changes in the ear drum. Histological degeneration of the ear drum occurs in the outer and inner fibrous layers of lamina propria and in the submucosal layer. These changes may reduce the elastic properties of the ear drum making it more susceptible to chronic perforation or retraction.
Genetics and race:
Incidence of COM varies in different population. The role of genetic factors playing a role in the pathogenesis of COM is rather difficult to elucidate with the present knowledge.
Environment:
Pollution and incidence of URI have a role to play in the pathogenesis of COM
Eustachean tube dysfunction and URI:
Eustachean tube dysfunction is more common in patients with COM. This is common in patients with skull base deformities.
GERD:
Secretions from the middle ear cavity was found to be rich in pepsiongen which could have come only from the stomach.
Allergy:
Predisposes to nasal block and eustachean tube dysfunction
Immune deficiency:
This is another probable cause for COM
Infection:
Mucopus from the ears of patients with COM is rarely sterile. Cultures frequently yield multiple organims and these vary depending on the climate, patient population and whether antibiotics have been given or not. Some studies have not found any differences in the bacterial composition between mucosal COM and squamosal COM.
Biofilms:
Biofilms have been identified both in active mucosal and active squamosal COM. Bateria exist as surface attached organizations. These organizations are known as biofilms. Biofilms have greater antimicrobial resistance, and host defences find it difficult to penetrate. These biofilms play a vital role in the pathogenesis of chronic infections.
Studies reveal that biofilms are present in 60% of patients with COM.
Examination of ear under microscope is the gold standard in the diagnosis of COM. Microscope allows the examiner to manipulate the ear, remove wax, clean up the secretions as both the hands are free. Ear drum can be visualized under magnification.
Otoscopy performed by using a microscope and appropriate aural speculum faciliates accurate diagnosis of COM. After a good aural toilet, the clinician can assess all areas of external ear and the ear drum.
Operation scars:
Prior to performing otoscopy the presence of operation scar should be looked out for in the post aural region / end aural region. This will help in accurately assessing the mastoid cavity if canal wall down surgery has been performed.
Mastoid cavities:
Cavities in the mastoid area could be created surgically or by the presence of cholesteatoma. Open mastoid cavities could be difficult to detect if the external canal is narrow or if the cavity is not continuous with the attic / antrum.
Site of the pathology:
This can be accurately described by visualizing the area of ear drum involved. In order to provide accurate description of the area of ear drum involved, the pars tensa is divided into 4 quadrants. They include:
Antero inferior
Postero inferior
Antero superior
Postero superior
Perforation of ear drum can be accurately described by describing the quadrants involved in the perforation.
In this condition hearing is impaired by the presence of permanent ear drum perforation. Since there no active infection / discharge hearing loss could be the only complaint.
These patients could benefit from myringoplasty / tympanoplasty / ossiculoplasty if needed.
Labyrinthitis:
Introduction:
This is defined as an inflammatory disorder involving the inner ear / labyrinth. Clinically this condition causes disturbances of balance and hearing of varying degrees in the involved ear.
Causes:
1. Bacterial infections
2. Viral infections
3. Autoimmune causes
4. Vascular ischemic causes
Pathophysiology:
Anatomically labyrinth is composed of an outer osseous framework surrounding the delicate membranous labyrinth which contains the peripheral end organs of hearing and balance. Membranous labyrinth include:
1. Utricle
2. Saccule
3. Semicircular canals
4. Cochlea
The labyrinth lies within the petrous portion of temporal bone. It communicates with the middle ear via the oval and round windows.
Infecting organism may find their way into the inner ear via:
Pre-existing fractures
Oval window
Round window
Congenital dehiscence involving the bony labyrinth
Viral labyrinthitis: Is characterized by sudden unilateral loss of hearing and equilibrium. Vertigo is usually incapacitating and associated with vomiting. These patients are bed ridden. Vertigo usually subsides within 4-6 weeks. Hearing loss is confined to high frequencies and is sensorineural in nature. An attack of upper respiratory tract infection precedes the development of labyrinthitis. This condition should not be compared with vestibular neuronitis which involves only the vestibular nerves and spares the cochlear component. Varicella Zoster oticus is an unique form of viral labyrinthitis caused by reactivation of dormant varicella zoster virus. This reactivated virus is known to attack spiral ganglion.
Common viral causes of labyrinthitis:
1. Mumps
2. Measles
3. Rubella (congenital labyrinthitis)
4. Cytomegalovirus
Bacterial labyrinthitis: can be potentially caused by meningitis / otitis media. This could be caused by direct invasion of membranous labyrinth by the infecting organism (suppurative labyrinthitis) causing permanent destruction of vestibular and cochlear end organs. In patients with meningitis spread of infections can be bilateral since infections can travel via the CSF and involve the inner ear fluids through the internal acoustic meatus / cochlear aqueduct. Bacterial infections involving the middle ear cavity can enter the labyrinth via erosion of lateral canal which is commonly seen in patients with cholesteatoma. Treatment is usually directed against infecting organism and supportive therapy. Suppurative labyrinthitis is usually followed by labyrinthitis ossificans where the whole of the membranous labyrinth gets ossified. Labyrinthitis ossificans indicates a permanently dead labyrinth.
Common bacterial causes of labyrinthitis include:
1. S. pnuemoniae
2. Haemophilus influenza
3. Streptococcus
4. Staphylococcus
5. Neisseria
6. Bacteroids
7. Proteus
8. Moraxella catarrhalis
Serous labyrinthitis:
This is a potentially reversible disorder caused by diffusion of bacterial toxins into the inner ear via the inflamed round window membrane. Studies have shown that the permeability of the round window membrane is increased when there is inflammation. This may cause diffusion of bacterial toxins and immune mediators into the inner ear causing transient impairment of the inner ear functions.
Brain abscess:
Otogenic brain abscess always develop in the temporal lobe or the cerebellum ofthe same side of the infected ear. Temporal lobe abscess is twice ascommon as cerebellar abscess. In children nearly 25% of brain abscessesare otogenic in nature, whereas in adults who are more prone to chronicear infections the percentage rises to 50%. The routes of spread ofinfection has already been discussed above, the commonest being thedirect extension through the eroded tegment plate. Although dura ishighly resistant to infection, local pachymeningitis may be followed bythrombophlebitis penetrating the cerebral cortex, sometimes theinfection could extent via the Virchow - Robin spaces in to thecerebral white matter. Cerebellar abscess is usually preceded bythrombosis of lateral sinus. Abscess in the cerebellum may involve thelateral lobe of the cerebellum, and it may be adherent to the lateralsinus or to a patch of dura underneath the Trautmann's triangle.
Stages of formation of brain abscess:
Stage of cerebral oedema: This is infact the first stage of brain abscessformation. It starts with an area of cerebral oedema and encephalitis.This oedema increases in size with spreading encephalitis. Walling off of infection by formation of capsule: Brain attempts to wall off the infected area with the formation of fibrous capsule. This formation of fibrous tissue is dependent on microglial and blood vessel mesodermal response to the inflammatory process. This stage is highly variable. Normally it takes 2 to 3 weeks for this process to be completed.
Liquefaction necrosis:Infected brain within the capsule undergoes liquefactive necrosis with eventual formation of pus. Accumulation of pus cause enlargement of the abscess.
Stage of rupture:
Enlargement of the abscess eventually leads to rupture of the capsule containing the abscess and this material finds its way into the cerebrospinal fluid as shown in the above diagram. Cerebellar abscess which occupy the posterior fossa cause raised intra cranial tension earlier than those above the tentorium. This rapidly raising intra cranial pressure cause coning or impaction of the flocculus or brain stem into the foramen magnum. Coning produces impending death. If the walling off process (development of capsule) is slow, softening of brain around the developing abscess may allow spread of infection into relatively avascular white matter, leading to the formation of secondary abscesses separate from the original or connected to the original by a common stalk. This is how multilocular abscesses are formed. Eventually the abscess may rupture into the ventricular system or subarachnoid space, causing meningitis and death.
The mortality rate of brain abscess is around 40%, early diagnosis after the advent of CT scan has improved the prognosis of this disease considerably..
The bacteriological flora is usually a mixture of aerobes and obligate anaerobes. Anaerobic streptococci are the commonest organisms involved. Pyogenic staphylococci is common in children. Gram negative organim like proteus, E coli and Pseudomonas have also been isolated.
Clinical features:
The earliest stage where the brain tissue is invaded (stage of encephalitis) is marked by the presence of headache, fever, malaise and vomiting. Drowsiness eventually follow. These early features may be masked by the complications such as meningitis or lateral sinus thrombosis. If this stage progresses rapidly to generalised encephalitis before it could be contained by the formation of the capsule, drowsiness may progress to stupor and coma followed by death..Usually the period of local encephalitis is followed by a latent period during which the pus becomes contained within the developing fibrous capsule. During this latent phase the patient may be asymptomatic.
During the next state (stage of expansion) the enlarging abscess first cause clinical features due to the alteration of CSF dynamics, and site specific features may also be seen due to focal neurological impairment. The pulse rate slows with rising intracranial pressure,the temperature may fall to subnormal levels. Drowsiness may alternate with periods of irritability. Papilloedema is also found due to elevated CSF pressure.
Clinical features also vary according to the site of involvement. Hence thedifferences that are seen between the cerebral and cerebellar abscess.
Cerebral (Temporo sphenoidal abscess):
A cerebral abscess in the dominant hemisphere often cause nominal aphasia, where in the patient has difficulty in naming the objects which are in day to day use. He clearly knows the function of these objects. Visual field defects arise from the involvement of optic radiations. Commonly there is quadrantic homonymous hemianopia,affecting the upper part of the temporal visual fields, more rarely it may also involve the lower quadrants. The visual field loss are on the side opposite to that of the lesion. This can be assessed by confrontation method. Upward development affects facial movements on the opposite side, and then progressively paralysis of the upper and lower limbs. If the expansion occur in inward direction then paralysis first affects the leg, then arm and finally the face.
Cerebellar abscess:
The focal features associated with cerebellar abscess is weakness and muscle incoordination on the same side of the lesion. Ataxia causes the patient to fall towards the side of the lesion. Patient may also manifest intention tremors which may become manifest by the finger nose test. This test is performed by asking the patient to touch the tip of the nose with the index finger first with the eyes open and then with the eyes closed. The patient may often overshoot the mark when attempted with the eyes closed in case of cerebellar abscess. The patient may also have spontaneous nystagmus. Dysdiadokinesis is also positive in these patients.
Investigations:
CT scan and MRI scans are the present modes of investigation. Scan is ideally performed using contrast media. These scans not only reveal the position and size of the abscess, the presence of localised encephalitis can be distinguished from that of an encapsulated abscess.Associated conditions such as subdural abscess, and lateral sinus thrombosis can also be seen.
Lumbar puncture: Isfrought with danger because of the risk of coning. Lumbar puncture mustbe performed in these patients only in a neurosurgical unit whereimmediate intervention is possible if coning occurs.
Treatment:
involves use of large doses of antibiotics. Ideally the abscess shouldbe controlled neurosurgically and with antibiotics. After the patientrecovers mastoidectomy is performed to remove the focus of infection.Abscess can be drained by placement of burr holes, and excision of thenecrotic tissue along with the capsule.
Thrombophlebitis can develop in any of the veins adjacent to the middle ear cavity. Of these the lateral sinus, which comprise of the sigmoid and transverse sinuses is the largest and most commonly affected. Initially it is usually preceded by the development of an extradural perisinus abscess. The mural thrombus partly fills the sinus. The clot progressively expands and eventually occlude the lumen.The clot may later become organised, and partly broken down and may even be softened by suppuration. During this stage there is a release of infecting organism and infected material into the circulation causing bacteremia, septicemia and septic embolisation.
Extension / propagation of the thrombus upwards may extend to the confluence of the sinuses, and beyond that to the superior sagittal sinus. Invasion of the superior and inferior petrosal sinuses may cause the infection to spread to the cavernous sinus. This spread of venous thrombophlebitis into the brain substance accounts for the very high association of this complication with brain abscess.Downward progression of thrombus into and through the internal jugular vein can reach the subclavian vein.
The harmful effects are caused by the release of infective emboli into the circulation, and also from the haemodynamic disturbances caused to venous drainage from inside the cranial cavity. The use of antibiotics have greatly reduced the incidence of lateral sinus thrombosis these days.
Formerly it was commonly associated with acute otitis media in childhood; now it is commonly seen in patients with chronic ear disease. In the preantibiotic era the commonest infecting organism was beta hemolytic streptococci. This organism was known to cause extensive destruction of red blood cells causing anaemia. Now a days the infection is by a mixed flora.
Clinical features:
These patients manifest with severe fever, wasting illness in association with middle ear infection. The fever is high and swinging in nature,when charted it gives an appearance of 'Picket fence'. It is always associated with rigors. The temperature rose rapidly from 39 - 40degree Centigrade. Headache is a common phenomenon, associated with neck pain. The patient appear emaciated and anaemic. When the clot extended down the internal jugular vein, it will be accompanied by perivenous inflammation, with tenderness along the course of the vein.This tenderness descended down the neck along with the clot, and would be accompanied by perivenous oedema or even suppuration of the jugular lymph nodes. Perivenous inflammation around jugular foramen can cause paralysis of the lower three cranial nerves. Raised intracranial pressure produce papilloedema and visual loss. Hydrocephalus could bean added complication if the larger or the only lateral sinus is occluded by the thrombus, or if the clot reaches the superior sagittal sinus. Extension to the cavernous sinus can occur via the superior petrosal sinus, and may cause chemosis and proptosis of one eye. If circular sinus is involved it could spread to the other eye. The propagation of the infected emboli may cause infiltrates in the lung fields, and may also spread to joints and other subcutaneous tissues..These distant effects usually developed very late in the disease, these could be the presenting features if the disease is insiduous in onset.Masking by antibiotics could be one of the causes. Patients always feel ill, and persisting fever is usual. The patients may have ear ache, in association with mastoid tenderness, and stiffness along the sternomastoid muscle. The presence of anaemia is rare now a days. Papilloedema is still a common finding. Other coexisting intracranial complications must be expected in more than 50 percent of patients. Extension of infected clot along the internal jugular vein is always accompanied by tenderness and oedema along the course of the vein in the neck, and localised oedema over the thrombosed internal jugular vein may still be seen. One rare finding is the presence of pitting oedema over the occipital region, well behind the mastoid process, caused by clotting within a large mastoid emissary vein, this sign is known as the Griesinger's sign. In fact there is no single pathognomonic sign for lateral sinus thrombosis and a high index of suspicion is a must in diagnosing this condition.
Investigations:
A lumbar puncture must be performed, if papilloedema does not suggest that raised intracranial pressure may precipitate coning. Examination of CSF is the most efficient way of identifying meningitis. In uncomplicated lateral sinus thrombosis the white blood count in the CSF will be low when the cause is chronic middle ear disease, and some what raised in acute otitis media. The CSF pressure is usually normal. The variations in the level of CSF proteins and sugar are not useful.