Tracheostomy
Contents
- 1 Definition:
- 2 History:
- 3 Indications of tracheostomy:
- 4 Advantages of tracheostomy:
- 5 Disadvantages of tracheostomy:
- 6 Types of tracheostomy:
- 7 Applied anatomy of trachea:
- 8 Surgical procedure:
- 9 Advantages of metal tracheostomy tube:
- 10 Decanulation procedure:
- 11 Tracheostomy in obese individuals with short neck:
- 12 Complications of tracheostomy:
- 13 Cricothyroidotomy:
- 14 Mini tracheostomy:
Definition:
The word tracheostomy is derived from the greek word tracheos plus stoma (mouth). This procedure involves creating an opening in the anterior wall of trachea with suturing of the skin of the neck with the tracheal mucosa. A tube is inserted through this stoma (opening) to facilitate respiration.
History:
It is one of the oldest described surgical procedure. It finds a mention in the Rig veda an ancient Hindu text of medicine (1500 BC).
Emperor Alexander was credited with performing the first tracheostomy. He is said to have performed this procedure on a soldier who chocked himself with his sword.
Jackson has been credited with documentation of tracheostomy as a modern life saving procedure. The number of tracheostomies preformed underwent a surge during the 18th and early 19th centuries due to diptheria epidemics which caused upper airway obstruction.
The advent of intensive care units and presence of ventilators during 1950s changed the status of tracheostomy from a life saving emergency procedure to that of a prolonged life supporting procedure.
Indications of tracheostomy:
"The main indication of tracheostomy is that when the surgeon thinks about it" (Mosher).
1. In upper air way obstruction (obstruction above the level of larynx). Trachesotomy is indicated in all cases of upper airway obstruction irrespective of the cause as an emergency life saving procedure. It is also indicated in impending upper airway obstruction as in the case of angioneurotic oedema of larynx.
2. For assisted ventilation: In comatose patients who donot have the required respiratory drive airway can be secured by performing a tracheostomy and the patient can be connected to a ventilator for assisted ventilation.
3. For bronchial toileting: Chronically ill patients who donot have sufficient energy to cough out the bronchial secretions may have to undergo tracheostomy with the primary aim of sucking out the bronchial secretions through the tracheostome.
4. In cases of prolonged intubation: tracheostomy will have to be performed to prevent subglottic stenosis.
Advantages of tracheostomy:
1. The procedure permanently secures the airway.
2. The anatomical dead space is reduced.
3. Tracheostomy byepasses the upper airway and hence it is useful in upper airway obstructions.
4. Suction can be applied through the tracheostome and bronchial secretions can hence be cleared.
5. If portex tube is used as tracheostomy tube it can be connected to a ventilator thus assisting the process of ventilation. The silastic tracheostomy tubes should not be sterilised using ethylene oxide because it has the ability to retain some to the gas for a period up to one week. The slow liberation of toxic bye products such as ethylene glycol and ethylene chlorhydrin can cause severe mucosal damage. These tubes have reduced the frequency of tracheostomy tube changes.
Disadvantages of tracheostomy:
1. It is a surgical procedure and hence has morbidity and mortality rates associated with surgical procedures.
2. The tracheostomy tube will have to be cleaned periodically.
3. During early phases periodical suction must be applied hence hospital support is a must.
4. The patient may not be able to use the voice. Some tracheostomy tube like the Fuller's metal tube may have a speaking valve which could help the patient to speak, the patient must get used to plugging the hole while speaking.
5. Decanulation is a complicated procedure.
Types of tracheostomy:
1. Temporary tracheostomy
2. Permanent or end tracheostomy - This is done in patients who have underwent total laryngectomy.
3. Mini tracheostomy
4. Percutaneous tracheostomy
5. Cricothyroidotomy
Applied anatomy of trachea:
The adult trachea measures 10 - 13 cms from cricoid cartilage to the carina (bifurcation of trachea). If the neck is extended roughly about half this length is within the confines of the neck making surgery easy. Hence tracheostomy is performed with the neck hyperextended. This is achieved by placing a sand bag or towel roll under the shoulder blade of the patient. In obese patients with short neck of elderly patient with scoliosis the trachea is entirely within the thorax making the procedure very difficult.
The shape of the trachea is maintained by the presence of incomplete cartilagenous rings. These rings extend anteriorly and laterally covering 2/3 of the tracheal dimension. Posteriorly trachea is lined by a membranous wall and trachealis muscle.
At the level of thoracic inlet the trachea dives anteroposteriorly behind thymus, innominate vein and innominate artery thus complicating tracheostomy procedure in elderly.
During dissection when one approaches the trachea in the midline it is found to lie under the following structures:
1. Platysma muscle
2. Superficial cervical fascia
3. Branches of anterior jugular vein
4. Sternohyoid, and Sternothyroid muscles.
5. Thyroid isthumus at the level of second tracheal ring
6. Pretracheal pad of fat through which inferior thyroid veins may wander, and sometimes thyroidea ima artery may be found in this plane.
The blood supply to the cervical portion of the trachea is derived from branches of inferior thyroid artery which enters the trachea laterally, hence during tracheostomy dissection is avoided in the area lateral to the trachea because it could compromise its blood supply. Blood supply to the trachea enters at the cartilage membranous junction. Recurrent laryngeal nerves also lie lateral to the trachea.
Surgical procedure:
Anaesthesia:
Under emergency situations it is performed under local infiltration anaesthesia. Under elective conditions it is performed under general anaesthesia.
Position: Supine with neck hyperextended.
Incision:
Emergency tracheostomy is performed with a vertical incision extending from the lower border of cricoid cartilage up to 2cm above supra sternal notch. This area is also known as the Burn's space and is devoid of deep cervical fascia.
Elective tracheostomy is performed through a horizontal incision at 2cm above the sternal notch.
If performed under emergency settings local anaesthesia is prefered. The drug used is 2 % xylocaine with 1 in 100000 adrenaline. 2 ml of this solution is infiltrated in to the Burns space.
Through a vertical incision extending from the lower border of cricoid cartilage up to 2cm above the sternal notch theskin, platysma, and cervical fascia are incised. Branches of anterior jugular vein if any are ligated and divided. Sternohyoid and Sternothyroid muscles are retracted using langenbachs retractors. The anterior wall of trachea is exposed after splitting the pretracheal fascia. The tracheal rings are clearly identified. Few drops of 2% xylocaine is instilled into the trachea through a syringe. This process serves to desensitise the tracheal mucosa while it is being incised. Incision over the trachea is sited between the second and the third tracheal rings. If the tracheostome is planned for a long duration then it is better to excise a portion of the tracheal ring completely. If tracheostomy is planned for a short duration of less than a month then the cartilage is not completely removed but partially excised creating a flap based either superiorly or inferiorly. This is known as the Bjork flap. This flap can be sutured to the skin to keep the tracheostome open. Trahceostomy tube is inserted into the opening and the wound is closed with silk.
A wet gauze is placed over the tracheostome in order to moisturise the inspired air.
If the patient is to be connected to a ventilator, then a portex tube is used. If the tracheostomy is performed to releive acute airway obstruction then a metal tracheostomy tube like the Fuller or Jackson is preferred.
Advantages of metal tracheostomy tube:
1. It is cheap
2. Easy to maintain
3. Patient will be able to speak by occluding the tube. This is possible in Fuller's tube because of the presence of speaking valve.
4. It is not irritating to the tracheal mucosa
5. Makes decanulation procedure easy.
Decanulation procedure:
The process of weaning the patient from the tracheostomy tube is known as decanulation. This process varies in adults and paediatric age groups.
Decanulation in adults:
If the patient is on portex tube then it should be changed into a metal one.
The opening of the tracheostomy tube is occluded using a spigget. Initially this spigetting is done during day time for 2 days. If the patient tolerates spigetting during day time for this duration then it is kept spigetted for full period of 24 hours. If the patient tolerates spigetting of this duration then the tube can be removed and the wound can be approximated and plastered. There is also the option of surgical closure of the tracheostome wound.
Decanulation in children:
Children easily get accoustomed to tracheostome. They also become dependent on tracheostome, this is due to the fact that a small child has a very poor respiratory reserve. So proper care must be taken while decanulating them. In children the tracheostomy tube is replaced by smaller and smaller sized tubes in 48 hour duration till the smallest size is reached after which complete decanulation is possible. The whole process could take atleast a week to complete.
Tracheostomy in obese individuals with short neck:
This is a really challenging scenario. The presence of excessive soft tissue in the neck prevents identification of landmarks. In short neck individuals the trachea is completely within the thorax.
The following procedures can be attempted in these patients:
1. Caudal distraction of shoulder
2. Taping of submental skin
3. Elevating the head of the patient by 30 - 45 degrees
4. Use of larger incision
5. Use of cricoid hook to pull the cervical trachea up into the neck from the thorax
6. The isthumus of thyroid if obstructing the field can be excised and ligated.
Complications of tracheostomy:
1. Injury to thryoid isthumus causing troublesome bleeding
2. Too lateral dissection may cause extensive bleeding and possible injury to recurrent laryngeal nerve.
3. Injury to the apex of the lung (right)
4. Sudden apnoea when the trachea is opened, due to loss of hypoxic respiratory drive. This can be prevented by slow opening of the trachea, or by subjecting the patient to inhage carbogen a mixture of carbondioxide and oxygen.
5. Subcutaneous emphysema if pretracheal fascia is not dissected properly, or too small a tube is introduced into the tracheostome.
6. Injury to great vessels. This can occur in children.
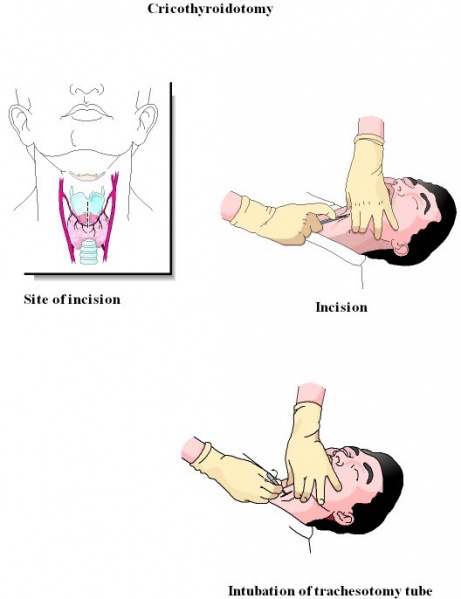
Cricothyroidotomy:
Is not performed commonly nowadays because of high incidence of postoperative subglottic stenosis. This procedure is indicated only under extremely emergency conditions.
Cricothyroid membrane is incised through vertical incision and tracheostomy tube is inserted through it. Ideally these patients must be converted into a regular tracheostomy within 48 hours.
Mini tracheostomy:
Here a small canula is passed through an opening made in the cricothryoid membrane. A separate mini tracheostomy kit is available for performing this procedure.
The kit contains:
1. A special scalpel
2. Canula
3. Obturator
4. Suction tube
5. A tape to anchor the tube
Indications include prophylactic and therapeutic indications.
Prophylactic indications:
After abdominal / thoracic surgical procedures the cough reflex is blunted predisposing to development of pneumonia. A mini tracheostomy in these patients will help in preventing pneumonia.
Therapeutic indications:
To clear sputum in patients with COPD, or in other conditions where there is sputum retention.
Contraindications:
1. Must be performed only by trained personal
2. If landmarks in the neck are not clear then this procedure should not be performed.
3. Should not be performed under extreme airway emergencies
The cannula when not needed can easily be removed and compression dressing can be applied over the wound.