Role of flaps in ENT
Contents
Introduction:
The term "flap" first originated during the 16th century from the Dutch word "flappe" meaning a structure that hung broad and loose, fastened only on one side.
Flaps are usually used to repair structural defects following surgery i.e. for malignant conditions of head and neck.
History:
Flap surgery dates as far back as 600 B.C., when Susrutha Samhita described nasal reconstruction using a cheek flap. In fact the origins of forehead rhinoplasty could be traced back to 1440 AD in India. Surgical procedures involving flaps during early phases involved the use of pivotal flaps, which involves transportation of skin to an adjacent area while rotating it about its pedicle (i.e. blood supply).
French surgeons were the first to describe advancement flap procedure, which involved transfer of skin from an adjacent area without rotation. Pedicled flaps were commonly used during the first and second world wars. In 1970's a clear cut distinction was made between axial and random flaps, muscle and musculocutaneous flaps.
It would be most inappropriate if the following persons are not remembered:
McGregor - Who introduced the forehead flap during 1963
Bakamjian - Who introduced the deltopectoral flap during 1965
Ariyan - Who pioneered the Pectoralis major myocutaneous flap in 1979
Daniel & Taylor - Who pioneered the free flap in 1973
Definition:
Flap is a unit of tissue that can be transferred from one site (donor) to another (recipient site) while maintaining its own blood supply. Flap is transferred with its blood supply intact, whereas a graft is a transfer of tissue without its own blood supply. Survival of graft depends entirely on the blood supply from the recipient site.
Classification:
Many different methods have been used to classify various types of flaps available. Almost all the classification systems can be divided under the following headings:
1. Blood supply
2. Tissue to be transferred
3. Location of donor site
Blood supply:
For any graft tissue to survive blood supply is a must. If the blood supply is derived from unnamed blood vessels then it is termed as "Random flap". Many local skin flaps fall in this category. If blood supply to the flap is derived from named vessel / vessels it is referred to as "Axial flap". Most muscle flaps fall in this category.
Fine tuning this classification category Mathes and Nahai further subclassified axial flaps into types I - V.
Type I Axial flap: Has only one vascular pedicle e.g. Facia lata
Type II Axial flap: Has blood supply served by dominant and Minor pedicles e.g. Gracilis flap
Type III Axial flap: Has blood supply served by two dominant pedicles e.g. Gluteus maximus flap
Type IV Axial flap: Has blood supply via segmental blood vessels e.g. Sartorious flap
Type V Axial flap: Derives blood supply from one dominant pedicle and many segmental blood vessels e.g. Latissmus dorsi flap.
Tissue to be transferred:
Flaps may be composed of just one type of tissue i.e. skin (cutaneous flaps), or may be composed of different types of tissue like skin, fascia and muscle. Classification can be made according to the type of tissue transferred.
1. Skin (cutaneous flap)
2. Fascia
3. Muscle
4. Bone
5. Viscera (colon, small intestine, omentum)
6. Composite : Fasciocutaneous, myocutaneous, tendocutaneous, and osseocutaneous flaps
Location of donor site:
Tissue could be transferred from an area adjacent to the defect. This type of flap is known as local flap. They may be further subclassified depending on its geometric design.
Pivotal flaps: are also known as geometric flaps. They include rotation, transposition, and interpolation types.
Advancement flaps: This type include single pedicle / Bipedicle / V-Y flaps
Tissue transferred from non contiguous site i.e. distant flaps. These flaps could either be pedicled or free flaps. The pedicled flaps are still attached to their blood supply, while free flaps are totally severed from their blood supply and are reattached to vessels at the recipient site (microanastomosis).
Principles of flap surgery:
Principle I : Replace like with like. This will go a long way in Camouflaging the surgical defect.
Principle II: Reconstruction should be thought in terms of units. It was Millard who divided the human body into 7 main parts (head, neck, body and extremities). He subdivided each of these parts into units. Each unit is further divided into subunits. These units and subunits should be considered and studied before the process of reconstruction is begun.
The most important aspect of these units are their borders. These borders include creases, margins and hair lines. Adherence to these borders during reconstruction is very important. It is always better to convert a partial unit defect into a whole unit defect before grafting. This will enable better consmesis.
Principle III: There should be a pattern and a fall back option always at hand.
Principle IV: The graft should be sutured without any tension. The donor area should not suffer excessive tissue loss.
All head and neck malignancies commonly present at an advanced stage. Surgical treatment always involve wide area of resection. This resected area will have to be grafted if the defect is large. Reconstruction of resected area is a very formidable task indeed.
The following are the common flaps used in the reconstruction following excision of head and neck tumors:
1. Pectoralis major myocutaneous flap
2. Deltopectoral flap
3. Radial forearm free flap
4. Temporalis flap
Pectoralis major myocutaneous flap:
Pectoralis major is a thick fan shaped muscle situated in the anterior chest wall.
The main arterial supply for pectoralis major myocutaneous flap is the pectoral branch of acromiothoracic artery, which arises from the first part of axillary artery. This vessel enters the muscle mass just below the clavicle near the junction of its middle and outer thirds. This is a pedicled flap. This represents the surface marking for the vascular hilum of the muscle. This flap is useful in reconstruction of defects in oral cavity, oropharynx, hypopharynx, and larynx.
This flap can be used to successfully reconstruct large defects, and is very versatile with a good survival rate because of its pedicled blood supply.
The following points should be borne in mind while elevating the flap:
1. The incision should be made above the nipple in male and below the breast in the female patient.
2. Pedicle should be identified carefully to preserve the vascularity of the flap
3. After repair of the defect rubber drains should be placed
Deltopectoral flap:
This flap was first described by Bakamjian in 1965. It is an axial flap designed on the anterior chest wall between the line of clavicle and the anterior axillary fold. This flap is supplied by perforating branches of internal mammary artery. Major advantage of this flap is that it can extend to any site in the neck even up to the level of zygoma. This flexibility is due to the fact that retraction of flap always occurs from side to side and not from end to end. This graft may hence elongate slightly over time, especially in old age patients.
This flap is outlined over the anterior chest wall and shoulder. The plane of elevation should be deep to pectoral and deltoid muscle fascia. Muscle fibers should be exposed as the flap is elevated. Elevation of this flap should only be done up to 2cms lateral to the sternal border taking care to avoid injury to perforating arteries. The donor site should be covered with split thickness skin graft.
Radial forearm free flap:
This is a fasciocutaneous flap based on radial artery. This flap as described has radial artery as its arterial source, venous outflow is from the superficial veins of forearm. Nowadays this is considered to be a workhorse for reconstruction in head and neck surgery. This flap is primarily used to reconstruct defects in the oral cavity, oropharynx and hypopharynx.
This flap included skin from the anterior cubital fossa to the flexor crease at the wrist. Skin should not be elevated over the ulnar artery.
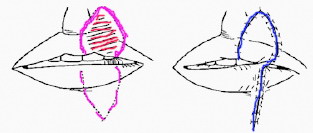
Abbe Estlander flap:
This flap is commonly used to reconstruct defects involving lips and commissures. Full thickness flap with skin / muscle / mucous membrane are used. A shield of incision is outlined with a minimum of 1 cm margin from the tumor. The flap can be marked, rotated and sutured leading to the formation of new commissure.
Nasolabial flap:
This flap is used to reconstruct the alar defect of the nose. The width of the flap should be slightly in excess of the size of the defect. Incorporation of blood vessel within the flap and defattening the flap will ensure better graft take.
The major advantage of this flap is that it is from the adjacent area, the skin thickness and color really matches the surrounding tissue.
Temporoparietal flap:
This flap is based on the superficial temporal artery. Both the anterior and posterior branches of superficial temporal artery should be included in the graft. The size of the flap should be approximately the size of the temporalis muscle. The arch of the zygoma should be fractured in order to deliver the graft into the oropharynx. The donor site could always be closed primarily.
Indications:
1. Coverage of large scalp defects
2. Oral cavity reconstruction
3. Reconstruction of nose
Glabellar flap:
This flap is commonly used to cover the facial defect over the bridge of the nose, eye lid reconstruction etc. This is usually a midline graft, wherein the flap is harvested from midline and is sutured into the defect.