Retropharyngeal abscess
Contents
Introduction:
Retropharyngeal abscess is a collection of pus between the posterior pharyngeal wall and the fascia and muscles covering the cervical vertebrae. It occurs in two forms - 1. The acute primary retropharyngeal abscess which is common in infants, and 2. Chronic retropharyngeal abscess which is common in adults. These two types of abscesses differ in their etiology and management.
Acute primary retropharyngeal abscess:
Is the more dangerous type occurring in infants. It is common between the age group of 3 months to 3 years. The predisposing factors are malnutrition, gastroenteritis, poor hygeine etc.
Etiology:
Abscesses may follow general debilitating illnesses like scarlet fever, measles etc. Infections from tonsils, adenoid and naso pharynx may even lead to the formation of retropharyngeal abscess. Rarely foreign bodies like bone pieces and pins may also cause retropharyngeal abscess.
Pathology:
The disease consists of suppurative lymphadenitis of the retropharyngeal nodes of Henle, situated on either side of midline between the psoterior pharyngeal wall and the aponeurosis over the bodies of the second and third cervical vertebrae. These glands receive the lymphatics of the post nasal space, pharynx, nose, eustachean tube and middle ear. These nodes atrophy between the 3rd and 5th year of life hence acute retropharyngeal abscess is uncommon in children above the age of 4.
The Henle's node when infected from the lymphatics, there is first adenitis, then periadenitis and abscess formation occur. The suppuration is usually one sided, and most prominent in the oro pharynx. If not evacuated in time or when it does not rupture, pus may spread along the esophagus or burst in different directions - towards the larynx, the angle to the jaw or even in to the external auditory canal. The pus is generally foul smelling yellow or whitish in color. It usually contains streptococci, and more rarely staphylococci and pneumococci.
Chronic retropharyngeal abscess:
Is commonly known to occur in adults. This is usually caused by tuberculosis. The tuberculous foci occur in the bodies of the cervical vertebrae( Pott's disease) which later spread into the retropharyngeal space. Primary syphilis of the mouth and pharynx may also cause retrophrayngeal abscess. This abscess usually is present in midline and is free to spread to either side also.
Symptoms:
These patients have excruciating pain while swallowing (odynophagia). Young infants with retrophryngeal abscess will refuse feed, may have extensive drooling. In adults the head may be held straight. Torticollis is also common in these patients. These patients may have difficulty in breathing (stridor), in which case tracheostomy must be considered to secure the airway in the first place. Constitutional symptoms like fever / toxicity is very common in acute retropharyngeal abscess.
Investigations:
Complete blood count show leucocytosis. Blood cultures can also be performed to ascertain the appropriate antibiotics to be used.
C reactive proteins are also found to increased in these patients
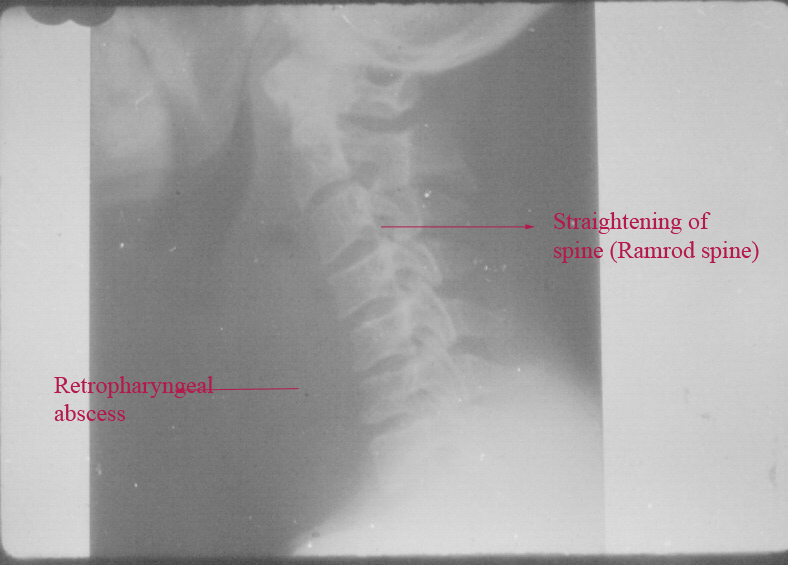
Xray soft tissue neck - A.P. and lateral views.
These pictures show prevertebral soft tissue widening. This can be ascertained by estimating the size of the prevertebral soft tissue which is normally half the size of the body of the corresponding vertebra. If the widening is more than half the body size of the corresponding vertebra then retropharyngeal abscess must be considered. The cervical spine are straightend with loss of the normal lordosis (Ram Rod spine). Above the prevertebral shadow air shadow is seen in almost all cases of retropharyngeal abscesses. This gas shadow is caused by entrapped air which occur during breathing. Some bacteria esp. Clostridium are known to form gases which may be entrapped in the prevertebral space.
C.T. scan neck or MRI study of neck will also help in clinching the diagnosis. This must ideally be performed using intravenous contrast agents. It appears as a hypodense lesion in the retropharyngeal space with ring enhancement. Other effects that could be seen are soft tissue swelling, and obliteration of normal fat planes.
C.T. scan is really helpful in differentiating cellulitis from abscess.
Management:
In majority of cases incision and draiuage is done and the pus is immediatly aspirated out using suction. The incision is made with 11 blade knife over the most prominent portion of the swelling. The I&D is done under local anaesthesia. In the case of infants it is preferable that the patient is held upside down while the surgery is being performed to prevent aspiration of pus into the lungs. When general anaesthesia is preferred a cuffed endotracheal tube must be used to minimize the hazard of aspiration of pus into the lungs. The patient must be put in Rose position (tonsillectomy position) while the I&D is being done to reduce the threat of aspiration.
When the abscess points towards the neck then it should be opened through an incision over the neck, preferably along the posterior border of sternomastoid muscle. The dissection is carried out behind the great vessels of the neck and in front of the prevertebral muscles. The surgery is followed by a course of antibiotics mostly cephalosporin group. Clinamycin in dose of 600-900mg intravenously 8th hourly can be administered in adults. Injection penicillin G in doses of 24 million units per day as continuous infusion along with metronidazole injection in doses of 500mg three times a day can also be considered. Metronidazole is highly effective against anaerobes.
If tuberculosis is suspected to be the cause then surgery is deferred. Anti tuberculous treatment is initiated.
Complications:
1. Mediastinitis
2. Airway obstruction
3. Atlanto occipital dislocation
4. Jugular vein thrombosis
5. Cranial nerve deficits especially the lower three ones
6. Haemorrhage secondary to involvement of the carotid artery