Recent trends in the management of frontal sinusitis
Contents
Introduction:
The size and the anatomy of frontal sinus is highly variable. It drains into the middle meatus via the killians infundibulum. This infundibulum opens in to the frontonasal recess. The drainage of frontal sinus is directed downwards, gravity assists its drainage. Because of this dependent drainage feature, acute sinus infections involving frontal sinuses heals fast and the patients respond well to conservative management.
Importance of frontal recess:
The width and the course of frontal recess is dependent on the size and number of anterior ethmoidal cells. Some of these cells may encroach into the frontal sinus (frontal cells, or frontal bulla). The more this frontal recess is curved, the more frontal cells develop into the frontal sinus. These cells obstruct the drainage from frontal sinus, causing acute sinusitis to become chronic. The presence of these frontal cells will mislead the surgeon into assuming he is already inside the frontal sinus when infact he has just opened the frontal cell.
Development of frontal sinus:
Frontal sinus is absent at birth. It begins to appear only at 6 months of age. Developmentally it arises from:
1. Direct extension of frontal recess
2. From one or more of anterior ethmoidal air cells
3. From the ventral extremity of ethmoidal infundibulum
It is this embryological origin which is responsible for the mucous patterns which may recirculate in the frontal recess along its medial wall.
History:
Headache caused by frontal sinusitis has a classic periodicity. It is more when the patient gets up from the bed in the morning and gets better as the day progresses. This feature is due to the beneficial effects of gravity assisted drainage.
Clinical examination:
Inspection & palpation: The anterior frontal sinus wall is examined for any signs of redness of skin / bulging. Tenderness may also be elicited by percussing the anterior wall of frontal sinus. This is a fairly reliable sign of acute frontal sinusitis. If percussion is painless in a patient with a bulge over frontal sinus then frontal mucocele should be suspected. Another way of eliciting frontal sinus tenderness is using the thumb to apply pressure over the floor of the frontal sinus. Pressure should be applied behind the supra orbital rim and not over the supra trochlear or supra orbital foramen, where tenderness could be easily elicited due to irritation of branches of supra orbital nerves.
Anterior rhinoscopy may not be useful to examine frontal sinuses. It is better to used angled telescopes to examine the frontal sinus recess area.
Role of Xray paranasal sinus:
Nowadays this is not acceptable as the only only imaging modality. This could be useful for templates to be cut in frontal osteoplastic surgical procedures.
CT scan of paranasal sinuses is the gold standard in the diagnosis of frontal sinusitis.
Anatomical variations of frontal recess plays a very important role in the pathogenesis of frontal sinusitis. Majority of cases of frontal sinusitis respond well to medications and conservative management. Surgery is indicated only in those intractable cases where there is long lasting obstruction to its drainage channel.
Various surgical approaches to frontal sinuses:
Frontal sinus trephination:
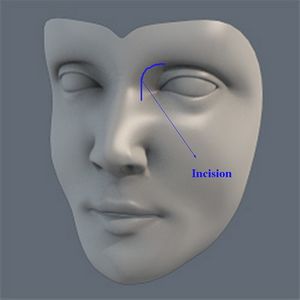
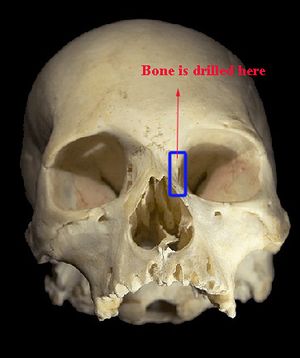
This is the oldest surgical intervention for acute purulent frontal sinusitis. A 1 cm incision is made just above the medial end of the eyebrow, and a small hole (0.5cm) is drilled over the anterior wall of the frontal sinus and the sinus cavity is entered. An endoscope may be used to examine the sinus cavity. Irrigation of the sinus cavity can be performed under endoscopic control. Irrigation should be done with extreme care if a defect of the orbital roof is seen on the CT.
External frontoethmoidectomy:
A slightly curved incision is made towards the medial canthus of the eye down to the level of the bone. This incision should divide the distance between the nasal dorsum and the medial canthus of the eye in the middle as shown in the figure.
The frontal sinus is opened up by resecting the lacrimal bone, part of the frontal process of maxilla and the frontal sinus floor.
The ethmoidal cell system should be dissected with care. The end result would be a single cavity encompassing the nose, ethmoids and frontal sinuses.
One basic conceptual error is encountered in this surgical procedure. Nearly 2/3 of the bony margins of frontal sinus drainage is resected in this surgical procedure causing excessive scarring. This could result in mucocele formation. Hence to avoid this potential complication, a stent should be left in place atleast for a period of 6 months.
Another important problem with this surgical procedure is the potential risk of injury to supra orbital and supra trochlear nerve. Patients also develop double vision postoperatively in 40% of cases.
Endonasal surgical drainage procedures:
Various types of endonasal surgical procedures are being practiced. These include:
Type I: Simple drainage procedure: This is accomplished endonasally by ethmoidectomy including the cell septa in the region of frontal recess. The inferior portion of killian's infundibulum and its mucosa is left undisturbed for fear of stricture developing. This procedure will be helpful when there is only a minor pathology in the frontal sinus, and the patient is free of risk factors like aspirin intolerance and asthma. These risk factors are associated with poor quality of nasal mucosa, causing unpredictable results. In majority of cases the frontal sinus heals spontaneously because of improved drainage.
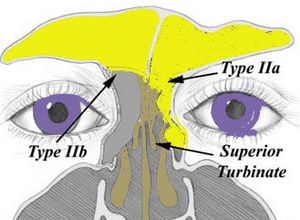
Type II or Extended drainage: This is of two types. Type IIa and Type IIb.
Type IIa: This procedure is performed by resecting the floor of the frontal sinus between the lamina papyracea and the middle turbinate.
Type IIb: This procedure is performed by resecting the floor of the frontal sinus between lamina papyracea and nasal septum anterior to the ventral margin of the olfactory fossa.
It has been assessed that the maximum size of the neoostium of frontal sinus that can be achieved in Type IIa procedure is 10 mm with a mean of 6mm. Somewhat larger opening can be created in Type IIb type of drainage procedure.
Preoperative CT scan may reveal the presence of socalled frontal cells. These are anterior ethmoidal air cells that has encroached into the frontal sinus giving a false impression that the frontal sinus has been properly opened. If these frontal cells are present, a procedure known as uncapping the egg is performed resulting in type IIa drainage.
Type III: (Endonasal median drainage)
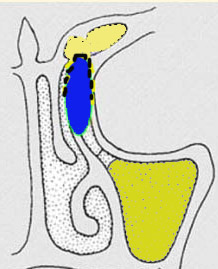
When frontal sinusitis is due to either bone or dense scar from prior surgery obliterating the communication of the frontal sinus to the nose, one approach to restoring drainage is to remove the entire floor of both frontal sinuses. This procedure is known as a type III frontal sinusotomy.
The elements of type III frontal sinusotomy are removal of the entire floor of both frontal sinuses, the intrasinus septum which divides the frontal sinus into a left and right cavity and upper nasal septum. To achieve the maximum possible opening of the frontal sinus, it would be helpful to identify the olfactory fibers on both sides. The middle turbinate is exposed and cut from anterior to posterior along its origin at the skull base. After cutting about 5mm the olfactory fibers could be seen coming out. This should be repeated on the opposite side also, resulting in a so called "frontal T". In performing this procedure both endoscope and microscope should be used.
In revision cases, type III drainage can begin from possible two points, from the lateral of medial side. The primary lateral approach is advisable if previous ethmoidal surgery was incomplete and the middle turbinate is still present as a landmark. Primary medial approach is justified if previous ethmoidal surgery was complete, and the middle turbinate is absent. The medial approach starts with the partial resection of the perpendicular plate of ethmoid of the nasal septum, followed by identification of the olfactory fibers on each side.
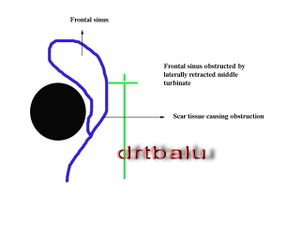
Frontal sinus rescue procedures: These procedures are indicated to clear up frontal sinus obstruction by laterally retracted middle turbinate and scar tissue. See figure below:
The scar tissue obstructing the frontal sinus drainage is resected first. After resection of scar tissue the remnant of middle turbinate becomes visible.
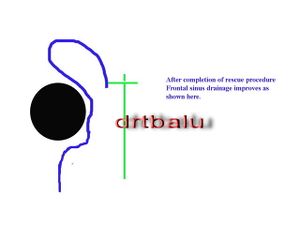
The medial osseous and mucosal lamina of middle turbinate are resected, the lateral mucosal lamina is preserved. This lateral mucosal lamina is turned medially
covering the skull base. The frontal sinus neoostium is epithelized.
Rhinofrontal sinuseptotomy:
Combined intra and extra nasal approach
This procedure is useful to manage difficult frontal sinus disease which has recurred even after repeated surgeries. This procedure was first developed by Stenert.
Surgical steps include:
1. External approach
2. Resection of frontal sinus pathology
3. Total resection of frontal intersinus septum
4. Partial endonasal resection of nasal septum
5. Bilateral subtotal resection of free dependent part of middle turbinate
6. Bilateral endoscopic ethmoidectomy
7. Enlargement of the isthumus area between both frontal sinuses and nasal cavities
8. Complete epithelization of neocommunication with free mucosal grafts.
Osteoplastic bone flap procedure is an external approach used in difficult inflammatory conditions involving the frontal sinus.
Indications:
1. Failure of Type III drainage procedure
2. Type III drainage procedure cannot be performed because the antero posterior diameter is less than 8mm
3. Laterally located mucopyocele
4. Major destruction of posterior sinus wall
5. Inflammatory complications following trauma
6. Correction of Pneumatosinus dilatans
7. Benign tumors involving frontal sinus