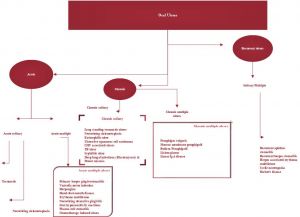
Lesions of oral cavity
Ulcers of oral cavity:
Ulcers involving oral cavity lining mucosa are rather common. Ulcers are characterized by defects in the epithelium, underlying connective tissue or both. Since the causative factors are so diverse the diagnosis of these lesions could be really challenging.
In order to differentiate acute from chronic lesions the following parameter is used:
If the ulcerative lesion lasts for two weeks or longer it is considered to be chronic; otherwise it is regarded as acute ulcer. Recurrent ulcers on the other hand present with a history of similar crops of lesions with evidence of intermittent healing.
The term solitary lesion indicates single ulcerative lesion, while the term multiple describes the presence of multiple ulcerative lesions. One common pitfall that should be avoided is not to miss a malignant ulcer diagnosis.
Causes of oral ulcer include:
Infection:
Viral infections:
Herpangina:
This is caused commonly by coxsakie viral infection. It commonly affects children. This is an acute febrile illness. Multiple small vesicles start to appear on the tonsillar pillars, tonsils, soft palate and uvula. These vesicles rupture to form ulcers which are about 2-4 mm in size. They usually have a yellow base with red areola surrounding them. They disappear within a period of 7 days.
Enterovirus 71 coxackievirus A16, and herpes simplex virus have been implicated.
Herpangina is generally a mild disease in adults, but infection during pregnancy has been associated with increased risk of low birth weight babies, preterm delivery.
These viruses spread via fecal oral route. They may also spread via respiratory route. Herpangina typically has an incubation period ranging between 4-14 days. The initial phase of viremia occurs after inoculation and results in distant sites of infection.
Clinical features:
Fever
Bilateral anterior, cervical lymphadenopathy
Inflammation of posterior pharyngeal wall
Persons with enteroviral infections may experience anorexia, emesis, abdominal pain which could mimic appendicitis.
Presence of skin exanthem is also noted. Patients with enteroviral infection may develop rashes that is not pruritic and it does not cause skin desquamation.
The charactersitics of skin rash include:
Macular
Maculopapular
Vesicular
Petechial
Hemangioma like
Herpetic gingivostomatitis:
This condition is also known as orolabial herpes. It is caused by herpes simplex virus. This is of two types:
Primary herpetic gingivostomatitis:
This affects children. It is characterised by clusters of multiple vesicles which ruptures to form ulcers. Any part of the oral cavity can be affected. Constitutional symptoms like fever, malaise, and head ache may accompany sore throat and lymphadenopathy.
Initial infection causes ulcers involving the gingiva. Herpetic gingivostomatitis is the most common cause of gingivostomatitis in children under the age of 5. It can also occur in adults.
Secondary / recurrent herpes:
Commonly affects adults. It is mild since adults have some immunity to this virus. Ulcers commonly involves the vermilion border of the lip (hence known as herpese labialis). Less commonly it can also involve the hard palate and gingiva. In recurrent herpes, it is presumed that the virus lies dormant in the trigeminal ganglion. When reactivated it travels along peripheral sensory nerves to involve the oropharyngeal mucosa.
Precipitating factors:
Emotional stress
Fatigue
Fever
Pregnancy
Immune deficiency status
Management:
Hydration is the most important component in the management of herpetic gingivostomatitis. Patients who are unable to maintain adequate hydration should be hospitalized. Acyclovir 200 mg five times a day for 5 days can be used to curtail the recurrence rates.
Hand, foot and mouth disease:
This is also viral infection affecting children. Oral lesions could be seen on the palate, tongue and buccal mucosa. Vesicles also develop on the skin of hands, feet and sometimes buttocks.
The viruses that cause this condition are coxsackie virus and enterovirus 71. A child can catch hand-foot-ane-mouth through contact with someone who already has this disease.
Bacterial:
Vincent's angina:
This is also known as acute necrotizing ulcerative gingivitis. This condition is caused by a fusiform bacillus and a spirochete - Borrelia vincentii. This condition commonly affects young adults and middle aged individuals.
This condition usually begins at the interdental papillae and then spreads to free margins of the gingivae which could become covered by necrotic slough. The gingivae could become red and oedematous. Ulcer and necrotic membrane can also form over the tonsil then this condition is known as vincent's angina.
Smear study from the affected area would clinch the diagnosis.
Management:
Systemic antibiotics which could include: Penicillin / Erythromycin and metronidazole. Frequent mouth washes with sodium bicarbonate solution could help. Scrupulus dental hygiene would also help.
Specific bacterial infections:
Tuberculosis, syphilis and actinomycosis could present with chronic oral ulcers. Oral tuberculosis lesions could be either primary or secondary. Primary lesions are rather uncommon and are seen in young patients. These ulcers are single and painless with regional nodal enlargement.
The seconday lesions are rather common and arfe associated with pulmonary disease. The oral lesions present as single indurated, irregular, painful ulcer covered by inflammatory exudates in patients of any age group. It is ofcourse common in middle aged and elderly patients. Oral tuberculosis may occur at any location on the oral mucosa, but tongue is most commonly affected. Other probable sites include palate, lips, buccal mucosa, gingiva, palatine tonsil and the floor of the mouth. Salivary glands, tonsils and uvula are also frequently involved.
Syphilis is a bacterial infection caused by Treponema pallidum. Clinical features of syphilis are diverse. It is characterized by cancrum and secondary mucocutaneous lesions. It may be associated with painless non-inflammatory bilateral satellite adenopathy of submandibular and cervical nodes.
Fungal infections:
Candidasis:
This is caused by candida albicans. It could occur in two forms.
Oral thrush:
This condition appears as white greyish patches on the oral mucosa and tongue. When wiped off they tend to leave an erythematous mucosa. This condition is seen in infants and children. Adults are affected when they suffer from systemic malignancy and diabetes, or taking broad spectrum antibiotics, cytotoxic drugs, steroids or irradiation.
Chronic hypertrophic candidiasis:
This is also known as candidal leukoplakia. It appears as a white patch which cannot be wiped off. Mostly it affects the anterior buccal mucosa just behind the angle of the mouth.
Thrush can be treated by topical application of nystatin / clotrimazole. Hypertrophic form may require excision.
Immune disorders:
Aphthous ulcer:
These are recurrent, superficial ulcers involving mobile mucosa (inner surface of lips, buccal mucosa, tongue, floor of the mouth and soft palate). It spares the mucosa of hard palate and gingivae. In its somewhat benign (minor) form (the commonest) ulcers are 2-10 mm in size and are multiple. There is a central necrotic area with a red halo. These lesions are self limiting and could heal within 2 weeks and does not leave a scar. In major forms of aphthous ulcer is very big, 2-4 cm in size and heals with a scar. It will be soon followed by another ulcer.
Aetiology of aphthous ulcer is unknown. It may be due to autoimmune pathology, nutritional deficiency (vitamin B12, folic acid and iron), viral, bacterial infection, due to hormonal changes.
Aphthous ulcers can be differentiated from viral ulcers due to their frequent recurrence, involvment of movable mucosa, absence of constitutional symptoms like fever, malaise and enlargement of lymph nodes.
Treatment includes topical application of steroids. Oral tetracycline has been used with some degree of success. Local pain can be releived by using lignocaine jelly.
Behcet syndrome:
It is also known as oculo-oro-genital syndrome. This condition is characterized by a triad of:
1. Aphthous like ulcers in the oral cavity
2. Genital ulcerations
3. Uveitis
The edge of the ulcer appears characteristically punched out. Lesions can also involve skin, joints and CNS.
Treatment depends on the individual patient, severity of the disease, and major organ involvement.
Theories behind the pathogenesis of this disease suggest an autoimmune etiology. It is thought that in genetically predisposed individuals exposure to an infectious agent / environmental antigen triggers autoimmune response.
Infectious triggers include:
Herpes simplex virus
Streptococcus species
Staphylococcus species
Escherichia coli
Involvement of multiple organs is observed in Behcet disease is due to the development of vasculitic / vasculopathic lesions in the affected areas. Microscopic evidence of inflammatory tissue infiltration with T cells and neutrophils have been demonstrated.
Criteria for the diagnosis of Behcet's disease as per Internation study group for Behcet's disease:
1. Recurrent painful genital ulcers that heal with scarring
2. Ophthalmic lesions which include anterior / posterior uveitis, hypopyon / retinal vasculitis
3. Skin lesions (erythema nodosum) like lesions
Management:
For managing oral / genital lesions topical steroids / sucralfate solution happens to be the first line therapy.
Colchicine has been used to prevent mucocutaneous relapse. To manage severe mucocutaneous lesions, systemic steroids, azathioprine, pentoxifyllne, dapsone have been used.
For management of ocular disease, azathioprine has beena accepted as the initial agent of therapy.
For managing GI lesions, sulfasalazine has been found tobe useful. Corticosteroids have also been used with reasonable degree of success in these patients.
Traumatic oral ulcers:
This is seen in the lateral border of tongue may be due to illfitting denture / jagged tooth, on the buccal mucosa due to cheek bite and the palate due to injury with a FB object like pencil / tooth brush. Acute ulceration of oral and oropharyngeal mucosa can result from accidental injestion of acids / alkalies.
Aspirin burn is seen in the buccal sulcus when a tablet of aspirin is kept against a painful tooth to get relief from tooth ache.
Oral ulcers due to neoplasm:
Malignancies involving the oral cavity and oropharyngeal mucosa present as chronic ulcers. Common malignancy involving oral mucosa is squamous cell carcinoma. Malignant neoplasms involving minor salivary glands can also present as oral cavity ulcers.
Skin disorders associated with oral ulcers:
Erythema multiforme:
This is a disease of rapid onset, and it involves the skin and mucous membrane of the oral cavity. The etiology is unknown, but may be associated with drug allergy (sulfanomides) or herpes simplex infection. Oral mucosal membrane consist of vesicles / bullae which ruptures to form ulcers which are covered with pseudomembrane. Lesions are common in the oral mucosa and tongue. These lesions cause bleeding. The most distinct feature of this disease is the presence of haemorrhagic cursts on the lips.
Skin lesions are seen on the palms, soles and exterior surface of the extremities. Oral lesions could occur without skin lesions in a quarter of these patients. Since these lesions are self limiting, management is purely supportive in nature.
Pemphigus vulgaris:
This is an autoimmune disorder which affects old age individuals. Oral lesions are seen in nearly half of these patients. In some patients oral lesions may actually precede skin lesions. Oral ulcers are superficial and involves palate, buccal mucosa and tongue. Treatment involves systemic steroids and cytotoxic drugs.
Benign mucous membrane pemphigoid:
This is an autoimmune disorder. Mucosal lesions involve cheek, gingivae, and palate. Conjunctiva is the next commonly involved site. Lesions begin as a bulla filled with clear / hemorrhagic fluid which ruptures to form superficial ulceration covered with shaggy mucosa. Skin lesions could be absent. Steroids are commonly used to manage these patients.
Lichen planus:
Oral lesions are seen in these patients. It could be with or without skin lesions. Skin lesions are usually pruritic, purple colored polygonal papules. Skin lesions are seen on the forearms and medial side of thigh. Oral lesions usually occur in two forms:
Reticular:
White striae lesions forming a lace like pattern are seen in the buccal mucosa on both sides. These lesions are asymptomatic and does not require treatment.
Erosive:
This condition is characterized by ulcers in the buccal mucosa, gingiva and lateral borders of the tongue. These lesions are rather painful. Each of these ulcers are surrounded by a keratotic periphery. Topical steroids are considered to be useful in managing these lesions.
Chronic discoid lupus erythematosis:
This condition is characterized by oral and skin lesions. Oral lesions are characterised by mucosal ulcerations which are painful in nature. These lesions are surrounded by keratotic periphery.
Drug allergy:
Systemic administration of drugs like penicillin, tetracycline, and sulfa drugs may cause erosive vesticular lesions in the oral cavity. Contact stomatitis can also occur due to exposure to mouth washes.
Vitamin deficiencies:
Vitamin B12 and folic acid deficieny can cause mucosal ulcerations in the oral cavity.
Radiation mucositis:
Oral ulcers can follow radiation of oral cavity for cancer. The oral mucosa first becomes red and then forms spotty areas of mucocitis which ultimately coalesce to form large areas of ulceration covered by slough.
Miscellaneous lesions of tongue and oral cavity:
Median rhomboid glossitis:
Introduction:
This condition affects the dorsum of the tongue. Usually it affects the junction between the anterior 2/3 and posterior 1/3 of the tongue. This is a chronic lesion about which very little is known. It usually appears as atrophic, erythematous, depapillated area.
Embryology:
Study of embryology of tongue will help us in understanding this disorder. Embryologically tongue is formed by fusion of two lingual tubercles with the midline structure known as tuberculum impar. Tuberculum impar arises from the first and second branchial arches. Sometimes the point of fusion between the lingual tubercles and tuberculum impar may be defective leaving a rhomboid area on the dorsum of tongue atrophic and devoid of papilla.
This area is highly susceptible to candidiasis. This area is usually erythematous. Erythema is usually caused due to inflammatory changes in the area. This lesion is commonly confused with erythroplakia which is premalignant.
Clinical features:
Median rhomboid glossitis occurs in midline of the tongue just posterior to the circumvellate papillae. Usually the lesion measures no more than 2cms in its greatest dimension. This lesion is more common in males. The lesion may appear whitish if there is excess keratin production. If there is associated candida infection, corresponding area of soft palate will show erythema. This phenomenon is known as kissing lesion.
This lesion is usually incidental in nature. If these lesions get infected by candida, then patients may have burning sensation when the patient eats.
Differential diagnosis:
This lesion should be differentiated from:
Lingual thyroid Tuberculosis Gumma of tongue Granular cell tumor
Histology:
Histological studies of this lesion demonstrate:
1. Atrophic stratified squamous epithelial lining 2. Moderately fibrosed stroma with dilated capillaries below squamous lining 3. Extensively elongated rete process are seen (possibly due to candida infection) 4. Silver staining may demonstrate candida hyphae
Treatment:
No treatment is usually necessary. If there is super added fungal infections then topical antifungal agents may help. Troublesome lesions can be resected totally.
Geographic tongue:
This condition is also known as benign migratory glossitis. This benign condition occurs in nearly 3% of general population. Majority of these patients are asymptomatic, but these patients are unusually sensitive to hot and spicy food. The etiopathogenesis of this condition are rather poorly understood.
This condition equally affects both sexes and are more prominent in adults than in children. Characteristic feature of geographic tongue is an area of erythema associated with atrophy of filiform papillae of the tongue. This is usually surrounded by a serpiginous white hyperkeratotic border. Activity of these lesions may wax and wane over time. These patients may occasionally be free of lesions.
Geographic tongue are common in patients with psoriasis.
These lesions are managed conservatively with supportive measures.
Hairy tongue:
This is a condition characterised by abnormal coating on the dorsal surface of the tongue. It is relatively common, temporary and really harmless condition affecting nearly 10% of the population. Even though hairy tongue can occur at any age it is frequent in older age group.
This condition is characterized by defective shedding of the tongue's dorsal covering tissue. This condition occurs due to lack of stimulation / abrasion to the dorsum of the tongue. This causes a build up of protein (keratin). In severe cases the length of these papillae are long resembling hair. If these papillae do not shed, food and bacteria can accumulate in the hair like mesh. Hairy tongue can assume any of these colors (brown, white, green or pink). The color depends on factors like the use of mouth washes and candy consumption.
Hairy tongue can be caused by:
Lack of oral hygeine
Use of antibiotics
Radiation treatment in the head and neck area
Excessive coffee / tea consumption
Tobacco use
Clinical features:
Buring sensation
Gagging / tickling sensation
Halitosis
Taste abnormalities
Figgured tongue:
It may be congenital or can be seen in patients with syphilis, vitamin B deficiency. Congenital fissured tongue with associated facial palsy is seen in patients with Melkersson-Rosenthal syndrome.
Tongue tie:
Tongue tie is diagnosed during physical examination. This is a rare (incidence 3-4%) and definite congenital abnormality. This can be identified by the fact that the tongue is anchored to the floor of the moth by a tight band of tissue.
Tongue is a highly mobile organ made up of longitudinal, horizontal, vertical and transverse intrinsic muscle bundles. The extrinsic muscles are the fan shaped genioglossus which is inserted into the medial part of the tongue and teh styloglossus and hyoglossus which insert in to the lateral portion of the tongue. Ths sublingual frenulum is a fold of mucosa connecting the midline of the inferior surface of the tongue to the floor of the mouth. In tongue tie the frenulum is actually thick, tight and short.
Tongue tie can be diagnosed in an infant who has difficulty in protruding the tongue over the lower lip and gum ridge. This commonly cause pain and soreness of nipple while the baby is breast fed.
Classification of Tongue tie:
Tongue tie is classified into 4 grades. Grades 1 and 2 are anteriorly attached frenulum while in grade 3 and 4 the frenulum is posteriorly attached.
Class I / Grade I tongue tie:
This is the real tongue tie and the tongue is classically heart shaped. The frenulum attaches to the tip of the tonge hindering tongue movement to a great extent.
Class II / Grade II tongue tie:
This is also considered as an anterior tongue tie. In this class the frenulum is attached just behind the tip of the tongue. The tongue is not heart shaped but the tongue tie is clearly visible.
Class III / Grade III tongue tie:
This is considered to be posteriorly attached frenulum. A thin membrane is seen in the frenulum, and this is the difference between class III and class IV.
Class IV / Grade IV tonge tie:
This is also a posterior tongue tie without the presence of thin membrane in the frenulum. These patients are able to elevate the front and sides of the tongue but the mid tongue cannot be elevated. This type of tongue tie is commonly missed.
Problems due to tongue tie:
1. Infants with tongue tie have difficulty in breast feeding as the mother will develop sore nipples because the child finds it difficult to attach its mouth to the nipple. This would result in the mother terminting breast feeding prematurely causing various problems to the child.
2. Speech defects can also occur due to tongue tie. This can cause dysarthria
Treatment:
This is indicated if the child has feeding problems
The child has speech problems (dysarticulation)
Surgery:
This procedure involves frenotomy or fenuloplasty.
Frenotomy:
This is a simple surgical procedure which can be performed with / without anesthesia. The doctor examines the lingual frenulum and uses a sterile scissors to snip the frenulum free. This procedure is quick and cause only minimal discomfort to the patinet. There are only few nerve endings and blood vessels in this area and hence there is relatively no pain or bleeding during the procedure. Even if bleeding occurs it is going to be only a few drops. The baby can be breast fed immediatly after the procedure.
Compllications:
1. Infection
2. Bleeding
3. Damge to sublingual salivary gland ducts
4. Scarring can reattach the tongue back to the floor of the mouth
Frenuloplasty:
This is a more extensive procedure needing anesthesia. General anesthesia is usually preferred in children. This procedure is indicated when the frenulum is too thick for frenotomy. The frenulum is cut using 11 blade or fine scissors. It is absolutely essential for the surgeon to get through the posterior component of the tongue tie for the procedure to be effective. The tongue tie that has been fully released has a diamond shaped wound. If there is no diamond shaped wound then the release is considered to be incomplete. The wound is closed with absorbable suture material like 3 -0 chromic catgut.
Fordyce spots:
These are aberrant sebaceous glands present under the buccal or labial mucosa. They shine through the mucosa as yellowish or yellowish-brown spots. This is seen with equal frequency in both males and females.
Nicotine stomatitis:
This condition is seen in smokers, particularly those in the habit of reverse smoking. Palatal mucosa shows pin point red spots in the centre of umbilicated papular lesions. This condition is due to the inflammation of the minor salivary glands and their duct openings as a reaction to the heat of the smoke. This condition is actually a misnomer as nicotine is not the cause. Elimination of smoking will help in releiving the symptoms.
Submucosal fibrosis:
Oral Submucosal fibrosis is a chronic debilitating potentially malignant condition of the oral cavity associated with betel nut chewing. It is characterized by fibrosis of the oral soft tissue, resulting in marked rigidity and inability to open the mouth. The inability to open the mouth is slowly progressive in nature.
History:
The term Submucosal fibrosis was first coined by Joshi in 1952. Su termed it as idiopathic sclerosis of mouth. Goleria in 1970 coined the term subepithelial fibrosis.
Pathophysiology:
Buccal mucosa was the most commonly involved site, but no part of the oral cavity is immune to this condition. Almost all the patients were pan chewers. Pathophysiology of this disease is not well established. A number of factors trigger the disease process by causing a juxtaepithelial inflammatory reaction in the oral mucosa. Factors such as areca nut chewing, ingestion of chilies, genetic and immunologic processes, nutritional deficiencies can lead to this condition.
Betel nut chewing: The areca nut component used along with betel leaf has been implicated. A recent study has clearly demonstrated the dose and frequency relationship of areca nut chewing in the pathogenesis of this disorder. Arecoline the active ingredient of areca nut is known to stimulate fibroblasts to increase its production of collagen by 150%. Flavinoids, catechin and tannin present in betel nuts cause collagen to cross link making them less susceptible to collagenase enzyme degradation. The disease process of Submucosal fibrosis is active even after cessation of betel nut chewing suggesting that arecoline not only affects the fibroblasts it also affects gene expression in fibroblasts causing them to produce increased amount of collagen with intense cross linkages.
Studies have also shown that arecoline inhibits metalloproteinases (particularly metalloproteinase 2) thus decreasing the overall breakdown of tissue collagen. Studies have also shown that keratinocyte growth factor-1, insulin like growth factor-1, and interleukin 6 expression, which have all been implicated in tissue fibrogenesis, were also significantly up-regulated by arecoline. Areca nuts are also rich in copper content. Chewing areca nuts increases the amount of copper in the oral cavity fluids. Copper is known to stimulate fibrinogenesis by activating copper dependent lysyl oxidase activity (suggested by Trivedi).
Ingestion of chillies in the pathophysiology has been controversial. Capsaicin the active ingredient of chillies have been demonstrated to increase the level of fibrosis in rats.
Genetic factors have also been postulated as the predisposing factor in the pathogenesis. Patients with submucosal fibrosis have been found to have an increased frequency of human leukocyte antigen A10 (HLA-A10), human leukocyte antigen B7 (HLA-B7), and human leukocyte antigen DR3 (HLA-DR3).
Immunologic process: have also been implicated in the pathophysiology of submucosal fibrosis. Increased levels of CD4 components have been demonstrated in these patients. The number of langerhan giant cells in the site have shown an increase.
Nutritional deficiencies: Iron deficiency, vitamin B complex deficiency, and zinc deficiency have also been postulated as predisposing factors. Infact these nutritional elements are necessary for normal repair mechanism to repair the oral mucosa which is constantly traumatized.
The morbidity and mortality of this condition is due to the fact that the patient is unable to open the mouth and consume normal quantities of food.
In Indian subcontinent females out number males in the incidence of this disease. No age group is immune to this condition. In Indian conditions in addition to the irritant effects of arecoline the nutritional deficiencies also play an important role in the pathogenesis of this disorder.
Clinical features:
1. Progressive inability to open the mouth due to fibrosis and scarring
2. Oral pain and burning sensation when the patient consumes spicy food
3. Increased salivation
4. Change in taste
5. Secretary otitis media due to stenosis of the pharyngeal end of Eustachian tube
6. Dryness of mouth
7. Dysphagia when consuming solids if esophagus is involved
Various stages of submucosal fibrosis are:
Stage I: Stomatitis, erythematous mucosa, vesicles, melanotic pigmentation of the oral mucosa, and mucosal petechia.
Stage II: Fibrosis begin with rupture of vesicles and healing of oral ulcers. Early lesions show blanching of the involved oral mucosa. Older lesions include vertical and circular palpable fibrous bands in the buccal mucosa and around the mouth opening or lips, resulting in a mottled marble like appearance of the mucosa because of the vertical, thick, fibrous bands running in a blanching mucosa. There is reduction of mouth opening in this stage, the tongue is stiff and small, the floor of the mouth has a blanched leathery appearance. The gingiva appears fibrotic and depigmented, the soft palate is rubbery with decreased mobility. The anterior and posterior pillars of the tonsils are pale and the tonsils also show atrophy. The uvula appear shrunken.
StageIII: Lekoplakia (premalignant condition) is a feature of this stage. Speech and hearing defects are also common in this stage
Khanna grouped these patients according to the degree of trismus to facilitate decision making regarding the management issues involved.
First degree: is the earliest stage. These patients do not have mouth opening difficulties. The only feature being the blanching seen in the oral mucosa associated with burning sensation on consuming spicy food.
Second degree: These patients have a mouth opening of 26 - 35 mm
Third degree: These are moderately advanced cases with mouth opening of 15 - 25 mm. Fibrotic bands are seen in the soft palate, anterior pillars of tonsils, and pterygo mandibular raphe.
Fourth degree: Most advanced case with severe trismus, presence of leukoplakia. This is infact a premalignant condition.
No specific lab study is indicated.
Histology:
Very early stage: is characterized by the presence of fine fibrillar collagen, marked oedema, large fibroblasts, large congested blood vessels with acute inflammatory reaction cells around it.
Early stage: is characterized by the thickening of the collagen bundles, increase in the number of fibroblasts and inflammatory cells.
Advanced stage: Collagen sheets form dense bundles, thick bands of subepithelial hyalinization occur in the submucosal tissue, there is decreased vascularity, and chronic inflammatory cells are seen. Chronic inflammation of minor salivary glands are also seen. This is the stage associated with severe trismus.
Treatment:
Medical: Weekly Submucosal intralesional injections of steroids may help in prevention of progression of the disease. Cessation of betel nut chewing is a must. Placental extracts can be injected intra lesionally to reduce the inflammatory effects of the disease. Use of topical hyaluronidase in doses of 150 units in association with steroids has proved beneficial.
Intralesional injection of IFN-gamma has a role due to the immuno regulatory effect of the molecule.
Surgical management is reserved only for advanced cases with severe trismus. This include excision of fibrous bands, with split thickness skin grafting.