Laryngeal complications of endotracheal intubation
Contents
Introduction:
William McEwen of England first performed orotracheal intubation in 1878. He used a tube made of brass. Endotracheal intubation to administer general anesthesia became common during first world war. Magill and Macintosh refined the process of general anesthesia. In 1964 PVC cuffed endotracheal tube was introduced. Initially they were low volume high pressure cuffed tubes. They caused lot of complications by way of vocal cord injuries. With the advent of high volume low pressure cuffed tubes in 1970 these injuries have been minimized.
Prolonged intubation:
Endotracheal intubation lasting for more than 2 weeks can be considered to be prolonged intubation. The first long term sequlae due to prolonged ventilation was first described by Bergstrom in 1962. He had used endotracheal intubation to treat patients with Barbiturate poisoning.
Indication for endotracheal intubation:
1. Temporary relief of upper airway obstruction
2. Assisted ventilation for respiratory failure
3. Pulmonary toileting
Advantages of intubation:
1. Major advantage of endotracheal intubation is the ease and rapidity with which the airway can be secured, hence it could be considered as the first step in securing the airway in times of crisis.
2. The whole procedure is reversible, and the tube can be removed without any problem.
3. Endotracheal intubation is used to administer anesthetic gases / oxygen during surgical procedures.
Pathogenesis of intubation induced injuries:
The endotracheal tube lies in the posterior portion of the larynx, hence the structures vulnerable to injuries are:
1. Mucous membrane and mucoperichondrium covering the medial surface of arytenoid cartilages and their vocal processes.
2. Cricoarytenoid joints and adjoining parts of cricoid cartilage below
3. Posterior glottic / interarytenoid regions
4. Supraglottic structures i.e. falsce vocal cords may become oedematous (reversible)
5. Tracheal injuries are uncommon with the advent of high volume / low pressure cuffs
6. Over inflation of cuff of endotracheal tube may cause mucosal injury and ciliary loss in trachea
7. Subglottic stenosis
Blood circulation in the mucosa and mucoperichondrium can be interrupted when the pressure from the endotracheal tube exceeds capillary pressure. This may cause edema / hyperemia / ulceration of mucosa / necrosis, ultimately leading on to erosion of perichondrium and cartilage.
Classification of intubation injuries:
Acute intubation changes:
General, Non specific:
Inflammation, edema, protrusion of ventricular mucosa
Pressure necrosis, loss of mucosa, cartilage and muscle
Glottic:
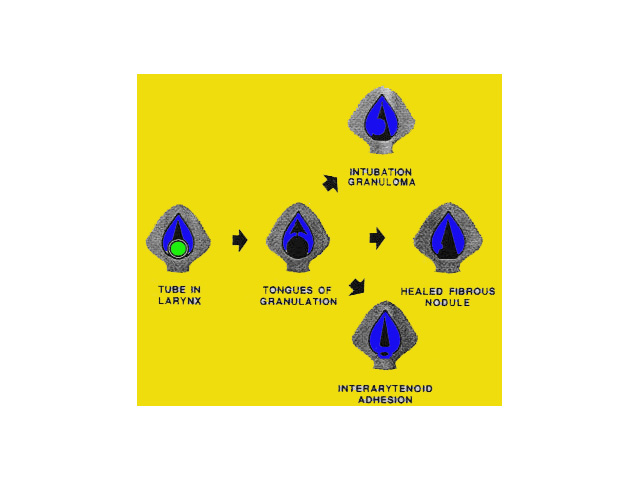
Flaps of granulation tissue
Granulation tissue
Ulceration of vocal process
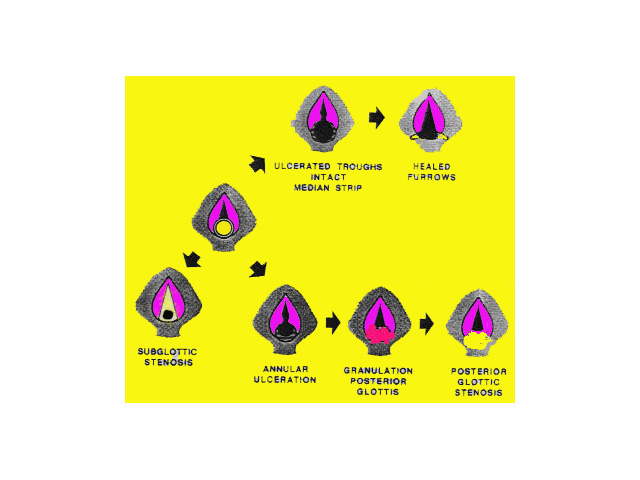
Ulcerated troughs and intact median strip
Posterior ulceration without intact median strip
Subglottis:
Bilateral posterolateral midcricoid ulceration
Annular inferior cricoid ulceration
Chronic long term complications:
General:
Submucosal fibrosis, scarring, stenosis
Ductal cysts
Glottic:
Granuloma, healed fibrous nodule
Healed furrows
Posterior glottic adhesion
Posterior glottic stenosis
Subglottic:
Posterior glottic stenosis
Circumferential subglottic stenosis
Types of intubation injuries:
Superficial ulceration: This is an early finding and can occur within hours of intubation. This is a potentially reversible condition and usually heals if the ETT is removed. Mild to moderate epithelial erosions usually heal by regeneration / re-epitheliazation.
Extensive ulceration: If ulceration is extensive, healing process is incomplete, and squamous metaplasia is commonly seen.
Perichondritis: If the necrosis penetrates the mucosa / mucoperichondrium to reach the cartilage, perichondritis occurs. This process may also lead to cartilage necrosis. Infection of ulcers also aggravate this process. With advancing cartilage necrosis the laryngeal framework may even become distorted. When ET tube is removed, healing occurs by second intention and fibrosis.
Factors responsible for laryngeal injuries:
Extrinsic factors:
Diameter, shape and contour of endotracheal tube: Safe sizes of ET tubes that can be used are 8mm in males and 7mm in females.
Plastic tubes of siliconized rubber: smooth-walled and less irritating
Duration of intubation: Adults 5-7 days, children 7-14 days are more prone
High volume low pressure cuffed tubes minimize risk of laryngeal trauma.
Traumatic intubation / multiple reintubations: Traumatic intubation can cause various complications. They include Hematoma, laceration, perforation due to use of excessive force, subluxation / dislocation of arytenoid cartilage.
Subsequent tracheostomy
Patient factors:
Poor tissue perfusion, sepsis, organ failure, malnutrition
Laryngopharyngeal reflux
Abnormal larynx: congenital stenosis, croup, crushed / burnt larynx
Wound healing, keloid formation
Preintubation status: Smoking causes increased risk of intubation induced granulomas
Movement:
During ventilator use
During application of suction
During coughing
During transport
Pathology:
Laryngeal edema and hyperemia follows irritation of laryngeal mucosa by endotracheal tube. Edema occurs very early during ET intubation. Supraglottic and glottic oedema very rarely causes permanent morbidity. Subglottic oedema especially in children usually causes airway obstruction.
Oedema usually occurs in the following areas:
1. Reinke's space
2. Ventricular mucosa causing prolapse of oedematous mucosa. This condition should not be confused with that of prolapse of ventricle which is a distinct entity.
3. Subglottic oedema. This condition usually resolves after extubation.
Granulation tissue:
Can be seen within 48 hours after intubation. This appears as pink soft vascular tissue. It commonly arises from the injured mucoperichondrium. Granulation involving the vocal process is the first pathology seen. The presence of granulation tissue should be considered to be a hall mark of healing process characterised by the formation of new blood vessels and the appearance of fibroblasts, inflammatory cells and collagen. Granulation tissue proliferates to involve the adjoining medial surfaces of the arytenoid cartilages. Some of the granulation tissue may be obscured by the presence of ET tube. They become evident only after removal of the tube.
Rarely flaps of granulation tissue may be seen to move with respiration, and if large and valve like it may cause laryngeal obstruction. In most of the cases removal of granulation tissue is not necessary. If granulation tissue must be removed it must be sent for culture to ascertain whether antibiotic treatment is necessary. Granulations commonly occur at the periphery of ulceration. Granulation tissue on long term basis may lead to granuloma formation, interarytenoid adhesion, or a healed fibrous nodule.
Management:
Most of the complications resolve after extubation. It is always better to convert ET intubation with a tracheostomy if the airway needs to be secured for a period of more than 2 weeks. This would definitely reduce the incidence of complications.
In the presence of unresolving oedema of vocal / vestibular folds then excision of the oedematous tissue may have to be resorted to. Resection is usually confined to one side in order to minimize incidence of adhesion formation. Extensive granulation tissue may similarly be removed endoscopically / laser excision.