Inflammatory disorders of thyroid gland
Introduction:
Inflammatory disorders of thyroid gland are a mixture of various disorders characterized by variable clinical presentations, etiologies and treatment modalities. These disorders cause the thyroid gland to be diffusely enlarged, nodular. Functionally speaking these patients may be euthyroid, hypothyroid or hyperthyroid. These patients may not suffer from pain except in cases of post viral and suppurative thyroiditis.
Inflammatory thyroiditis are often associated with certain characteristic triggering factors:
1. Parturition
2. Viral infections
3. Medications
Classification of inflammatory thyroid disorders:
This takes into account the subjective history (painful or painless), its temporal course (acute, subacute or chronic), histopathologic features (hyperplastic, lymphocytic, granulomatous, or fibrous), and the name of the physician who first described them (Graves, Hashimoto, DeQuervain, and Riedel). These parameters cause a lot of confusion when classifying this disorder.
A simple classification of inflammatory thyroiditis has been evolved. It divides the various disorders into four main groups:
1. Autoimmune
2. Amiodarone induced
3. Infectious
4. Idiopathic
Autoimmune thyroid disease:
This is the commonest of inflammatory thyroid disorders. Disorders under this group include:
a. Hashimoto's thyroiditis (Chronic lymphocytic thyroiditis)
b. Subacute lymphocytic thyroiditis
c. Postpartum thyroiditis
d. Grave's disease
This group of disorders is characterized by immune reaction against thyroid autoantigens. There are three serologic markers for disorders belonging to this group.
They are:
1. Antibodies against thyroid globulin (the large protein on which T3 and T4 are synthesized and subsequently cleaved)
2. Thyroid microsomal antigen (also known as thyroid peroxidase)
3. Thyrotropin receptor
The presence of thyroid antibodies facilitates lymphocytic infiltration of the thyroid gland which is a feature of autoimmune thyroiditis. If thyroid receptor stimulating antibody is present, it can cause hypertrophy of the gland with minimal lymphocytic infiltration. This picture is seen in Graves disease. Autoimmunity also can induce a thyrotropin receptor antibody which blocks normal thyrotropin from activating it causes hypothyroidism without lymphocytic infiltration. Autoimmune thyroid disease may present either with thyroiditis or as a hyperplastic disorder i.e. Graves disease. When a clear precipitating factor could be associated with this disorder then it could be used to name the subtype of the disorder i.e. (Postpartum thyroiditis, interferon induced thyroiditis) etc. Sometimes these various subtypes of autoimmune thyroiditis could be seen in the same patient.
Hashimoto's thyroiditis: is the most common inflammatory disorder of thyroid gland. Patients present typically with goitre, nodules, with hypothyroidism. High titres of circulating thyroid antibodies is a feature of this disorder.
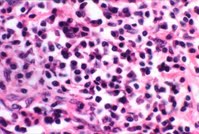
Histologically, the gland shows follicular degeneration with a diffuse lymphocytic infiltration. There may also be associated fibrosis. These features are identifiable in FNAC. If there is palpable cervical node associated with Hashimotos thyroiditis then FNAC of thyroid should be performed to rule out malignancy.
Subacute lymphocytic thyroiditis: This disorder comprises of three subtypes. They are Postpartum thyroiditis, silent thyroiditis and interferon induced thyroiditis. All these three subtypes have positive microsomal antibodies.
Postpartum thyroiditis: affects 5% of females. Women with positive thyroid antibodies during the first trimester of pregnancy have roughly 50% chance of developing postpartum thyroiditis. Hyperthyroidism usually develops during the first three months following delivery. It is usually mild and may last for a few months. The patient may then become euthyroid and later hypothyroid. These patients commonly have a mild to moderately enlarged thyroid gland. TSH levels may be raised. Antithyroid drugs are not indicated in these patients on the other hand steroids may have a role to play. Silent thyroiditis has no clear cut precipitating risk factors. Silent thyroiditis may precede or succeed other types of autoimmune thyroiditis. The diagnosis is usually one of exclusion. Interferon a commonly used immunoactivating agent in the treatment of viral hepatitis can cause thyroid dysfunction. Pre existing auto immune thyroiditis is considered to be a risk factor in the development of interferon induced thyroiditis. This type of thyroiditis is generally mild and self limiting.
Graves disease:
is an autoimmune disorder involving the thyroid gland. It also carries with it the risk of developing other subtypes of autoimmune thyroiditis.
The classic presentation of Graves disease include:
1. Hyperthyroidism 2. Goitre
3. Opthalmopathy
4. Dermopathy (unusual)
5. Acropachy
Tests used to diagnose Graves disease:
Serum TSH estimation (elevated)
Total or free T4 assessment
Presence of microsomal antibodies
Radioactive iodine uptake
Hyperthyroidism in Graves disease is caused by activating thyroid stimulating antibody against the thyrotropin receptor. There is also an increased incidence of thyroid carcinoma in these patients.
Treatment: In the short term these patients can be managed with antithyroid medications. Long lasting effects can be produced with ablation of gland function by 131I administration, followed by life long supplements of thyroid hormones.
Surgical ablation of the gland is another option. Before embarking on it the patient should be made euthyroid by use of antithyroid drugs. Oral administration of Iodine should be discouraged in these patients unless and until the patient has been started on antithyroid drugs.
Radioactive iodine uptake studies:
| RAIU | RAI Scan | |
|---|---|---|
| Inflammatory thyroiditis | Low | Minimal trapping |
| Toxic multinodular goitre | Normal to high | Cannonball pattern |
| Grave's disease | High | Homogenous / diffuse |
Amiodarone induced thyroiditis:
Amiodarone is a potent antiarrhythmic drug. This drug is structurally related to thyroxine. It initially causes hyperthyroidism which is unwelcome in cardiac patients. The types of thyroid dysfunction caused by amiodarone is as follows:
Type I: This type behaves like toxic multinodular goitre or graves disease with normal or high radioactive iodine uptake. It responds well to antithyroid medications.
Type II: Behaves like chemical thyroiditis and is responsive to steroids. Diagnostic tests to clinch the diagnosis include:
1. TSH estimation
2. Free T3 T4 estimation
3. Microsomal antibodies
4. Radio active iodine uptake scan
Management:
In most of the cases it is necessary to discontinue the drug. Thyroidectomy may be considered in patients who need to continue taking amiodarone because of their heart condition.
Infectious thyroiditis: Is commonly caused by viral infections. Post viral thyroiditis is also known as De Quervain's disease, whereas bacterial thyroiditis tend to suppurate. Suppurative thyroiditis is painful.
Fibrous thyroiditis: Also known as Riedel's thyroiditis. This is a very rare entity causing fibrosis of thyroid gland and surrounding tissue. Etiology is unknown. It is associated with retroperitoneal fibrosis, pseudo tumor of orbit and sclerosing cholangitis. Majority of patients are women in the fifth decade of life.
Diagnosis involves use of biopsy. In cases of tracheal compression, excision of isthmus will suffice. Otherwise it is a self limiting disease. Medical therapy includes glucocorticoid administration. Tamoxifen could also be used.