Evalutaion methadology of lacrimal apparatus and orbit
Contents
Introduction:
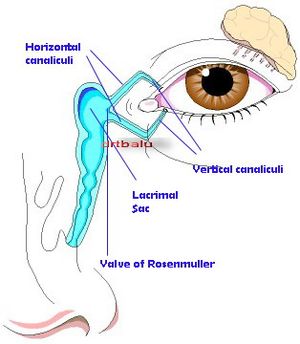
Tears which are produced by the main and accessory lacrimal glands are mostly drained by the lacrimal drainage system. Any disorder affecting the lacrimal system causes the complaint of tearing (epiphora). Excessive tearing could be caused by hypersecretion from the tear glands or insufficient drainage of tears through the lacrimal drainage system. In this article we will be evaluating the various evaluation methodologies available to study lacrimal and orbital disorders.
Role of History taking:
This is the most underestimated but a very important aspect of evaluation methadology. Patient should be queried with intention of identifying whether epiphora is cased secondary to overproduction of tears or due to inefficient drainge of the secreted tears.
In epiphora due to overproduction of tears, the problem will be bilateral, and is associated with minimal eye discharge or crusting. Tearing due to insufficient drainage by contrast will be mostly unilateral, and is associated with eye discharge and crusting. Crusting will be more evident on getting up from sleep. In patients with complete obstruction of lacrimal drainage system, infection commonly develops in the lacrimal system causing swelling, redness, and tenderness in the medial canthal region. Lacrimal sac infections (dacryocystitis) is associated with pain around the eye. In pediatric patients this may progress to orbital / periorbital cellulitis.
Clinical examination:
The aim is to confirm infromation obtained in the history. It also helps in evaluating which segment of the lacrimal drainage apparatus is obstructed.
The examination includes:
1. Inspection of the eyelid position, contour and function in relation to the operation of the lacrimal pump. Malpositions of eyelid such as ectropion, where in the punctum is not apposed to the globe will always be associated with epiphora.
2. Facial nerve palsy may lead to paralytic ectropion / weakness of orbicularis muscle. Weakness of orbicularis oculi may affect the lacrimal pump mechanism. Contractions and relaxations of orbicularis oculi is neccessary for tears to be pumped into the lacrimal sac.
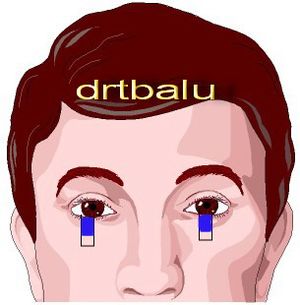
3. Punctal abnormalitis: This condition sould be carefully looked for. Punctal ectropion may be associated with epiphora. Each punctum should be assessed for patency. Normal punctum is usually 0.3 mm in diameter. Congenetial / acquired stenosis of the punctum may interfere with tear drainage mechanism. Swelling / erythema around the punctum may signify canaliculitis. In these cases pressure over the canaliculus may cause tear reflux, while pressure over lacrimal sac area does not show any reflux. The canalicular area should be palpated carefully to seek evidence of calculi.
4. Palpation over the medial canthal area may reveal a mass in the area of lacrimal sac, in patients with significant lower tear drainage channel obstrution. Lacrimal sac tumors must be diligently excluded by palpating this area. In patients with significant lower lacrimal drainage channel obstruction, palpation over lacrimal sac area will cause pain with reflux of tears / secretions / pus. If the reflux is purulent then significant dacryocystis should be suspected.
5. Intranasal examination: This is a must. All suspected patients should undergo diagnostic nasal endoscopic examination to rule out sinonasal causes of lacrimal outflow obstruction.
6. Slitlamp examination: Will reveal elevation of precorneal tear film.
7. Diagnostic tests: Many tests have been designed to localize obstruction in the lacrimal outflow system. These tests either individually or in combination is useful in the diagnosis.
Schirmer's test:
This test is basically prepared to quantitate tear production. This test is performed by placing strips of white filter paper at the junction of the middle and lateral thirds of the lower eyelids after administration of a topical anesthetic agent. The tear production is measured with the eyes closed. Produced tears will wet the filter paper. The length of the filter paper which becomes wet is assessed at the end of 5 minutes. Normal test result is between 10mm and 30 mm of wet filter paper. Normally it should not exceed 30 mm. A value of more than 30 mm is considered to be epiphora. A value of less than 10 mm is considered to be dry eye (hyposecretion).
Fluorescein dye disappearance test: This test can be easily performed as an office procedure. The steps are as follows:
A mixture of topical anesthetic and flurescein dye is placed in the inferior fornix of each eye. The tear film formed in each eye is observed and compared over a period of 5 - 10 minutes. This dye should drain rapidly through a patent lacrimal drainage system. Persistence of dye in the tear film even after 10 minutes indicates abnormal lacrimal outflow. This could be due to functional / anatomic obstruction in the lacrimal drainage apparatus.
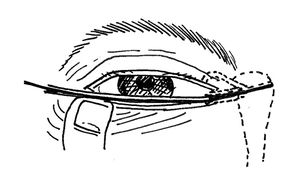
Punctal dilatation and canalicular probing:
This simple test is used to evaluate patency of the proximal ductal system. Difficulty with dilatation may indicate clinically significant punctal stenosis. Similarly difficulty with probing through the canaliculus may indicate canalicular stenosis / stricture. This is a contraindication for endoscopic dcr. Drainage may improve if probing opens up the stenosed canaliculi. Easy probing up to the superior portion of lacrimal sac is a good indicator of upper lacrimal drainage pathway patency.
Lacrimal irrigation:
This test is used to diagnose the location and extent (complete / partial) of an obstruction. A 23 - 27 gauge cannula is attached to a syringe containing sterile saline solution. This is introduced into the proximal canaliculus (usually the lower one) following punctal dilatation. Irrigation should be performed in both eyes even in patients with unilateral epiphora, since the normal eye can be used as the basis of comparison. In the presence of patent / partially patent lacrimal system the saline finds its way into the nasal cavity. Reflux of the injected saline through the same punctum indicates canalicular obstruction, while reflux from the opposite punctum indicates obstruction distal to the common canaliculus. Distention of lacrimal sac or reflux of purulent secretion indicates nasolacrimal duct obstruction. Reflux of bloody fluid indicates lacrimal system inflammation, a lacrimal sac tumor, or trauma to the tissues while introducting the cannula.
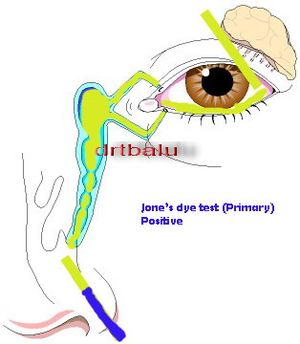
Jones dye tests:
This group of tests are used to distinguish between functional and anatomic outflow problems. The primary test is performed by placing topical anesthetic and flurescein dye into the conjunctival sac. Topical 4% xylocaine and oxymetazoline nasal sprays may be used to anesthetize and vasoconstrict the inferior meatus of the nose. A cotton tipped applicator is placed beneath the inferior turbinate near the opening of the nasolacrimal duct. Recovery of fluorescein dye in the nose indicates a functionally and antomically patent system. Non recovery of the dye (negative result) suggests a functional or anatomic blockage.
In the event of negative dye test, secondary dye test should be performed. This test is performed after removal of residual fluorescein from the conjunctival sac. Clear saline solution is placed into the inferior canaliculus using a syringe / cannula. The irrigant is retreived from the nasal cavity by tilting the patient's head forward over a basin. If fluoresein dye is present in the irrigant (positive result) then it is assumed that the upper lacrimal system is functional while the lower system is partially open and is not functional. Recovery of a clear irrigant (negative result) indicates a functional problem with the upper system.
Dacryocystogram:
This test helps to evaluate the anatomy of the lacrimal system. In this test contrast medium is injected into the lacrimal system through the lower canaliculus, and performing a serial radiography. The anatomy of the complete outflow system becomes visible. This test is useful in identifying congential anamolies involving the lacrimal outflow tract.
Evaluation of orbit:
This must serve to distinguish orbital from periorbital, intraocular and sinonasal disorders. The most commonly encountered orbital disorders of interest to an otolaryngologist are 1. Grave's disease and 2. Orbital fractures.
Grave's disease:
Also known as Thyroid eye disease is diagnosed in the presence of hyperthyroidism. The irony is that it could be present even in euthyroid or hypothyroid patients.
Criteria for diagnosis of thyroid eye disease:
1. Presence of eyelid retraction: This is one of the major criteria. In the presence of eyelid retraction the diagnosis can be made in the presence of one of the following: Thyroid dysfunction, exophthalmos, optic nerve dysfunction or extraocular muscle involvement.
2. In the absence of lid retraction, the diagnosis can be made in the presence of thyroid dysfunction along with one of the following: exopthalmos, optic nerve dysfunction, or extraocular muscle involvement.
Presenting symptoms:
1. Ocular irritation / discomfort
2. Conjunctival injection / tearing
3. Diplopia
4. Proptosis
5. Lid retraction
When proptosis is symmetrical the patient may miss it.
Extraocular muscle inflammation and enlargment in Grave's disease my limit eye movement and cause double vision. Eye muscle function can be evaluated by determining the alignment of the globes in the primary position and accessing its mobility. Cover - uncover test will reveal even mild misalignments.
Observation of upper eyelid movement may be helpful in the evaluation of thyroid eye disease. Normally, upper eye lid descends smoothly and competely with downward rotation of eye as seen in downward gaze. When this movement is delayed or incomplete then it is known as the lid lag, which is a feature of thyroid eye disease.
Lagophthalmos: is defined as incomplete closure of eyelids. This is commonly seen in thyroid eye disease.
Proptosis: Is defined as forward protrusion of eyeball. This can be measured using an exopthalmometer.
Orbital fractures:
Symptoms include:
1. Pain
2. Diplopia (commonly seen in blow out fractures)
3. Facial numbness
4. Trismus
5. Periorbital oedema
6. Ecchymosis
7. Orbital emphysema
8. Hypoesthesia of cheek and upper lip (seen in fractures of orbital floor)