Complications of Otitis media
Contents
- 1 Introduction:
- 2 Intracranial complications:
- 3 Route of spread of infection from the ear:
- 4 Factors that determine the spread of infection:
- 5 Extradural abscess:
- 6 Clinical features:
- 7 Management:
- 8 Lateral sinusthrombosis:
- 9 Queckenstedt test:
- 10 CT scanning:
- 11 Angiography:
- 12 Arteriography:
- 13 MRI:
- 14 Meningitis:
- 15 Brudzinski's sign:
- 16 Brain abscess:
- 17 Cerebral (Temporo sphenoidal abscess):
- 18 Cerebellar abscess:
- 19 Otitic hydrocephalus:
Introduction:
Complications of otitis media occur as a result of infection spreading from the mucosa of the middle ear cleft to the adjacent structures. Usually the middle ear space is separated from adjacent structures by bone. During preantibiotic era complications commonly followed acute otitis media. With the advent of antibiotics it the chronic otitis media which is causing complications .
Even though the incidence of these complications have drastically reduced after the advent of potent antibiotics, the morbidity and mortality caused by the complications are still very high.
The complications of otitis media fall under two categories:
1. Complications within the cranium
2. Complications within the temporal bone
Intracranial complications:
These can be further subclassified into extradural and intradural complications.
Extradural complications:
. Extradural abscess
. Meningitis
. Sigmoid sinus thrombosis
Intradural complications:
. Subdural abscess
. Brain abscess
. Otitic hydrocephalus
Intratemporal complications:
. Facial palsy
. Labyrinthitis
. Petrositis
. Subperiosteal abscess
. Internal carotid artery aneurysm
Extratemporal complications :
. Subclavian vein thrombosis
. Luc's abscess
. Citelli's abscess
. Bezold's abscess
Route of spread of infection from the ear:
Whether acute or chronic, the infection from the middle ear spreads via:
1. Extension through bone that has been demineralised during acute infections, or resorbed by cholesteatoma, or osteitis in chronic disease of the ear. Demineralisation is brought about by various enzymes that are released during the acute infections. Cholesteatoma causes bone erosion either due to pressure necrosis, or halisterisis. Halisterisis is also known as hyperimic decalcification. As the term itself suggests decalcification is caused by hyperaemia.
2. Spread through venous channels:
Spreading of infected clot within small veins through the bone and dura into the dural venous sinuses. If spread via this route occurs then the infection may find its way into the brain without involving the bone or dura. Thrombophlebitis from the lateral sinus may spread to the cerebellum, and from the superiorpetrosal sinus may spread to the temproral lobe of the brain.
3. Spread through normal anatomical pathways: Spread may occur through oval / round windows into the internal auditory meatus. Spread may also occur through the cochlear and vestibular aqueducts. Certain areas may have dehiscent bone as a normal variant i.e. bony covering of the jugular bulb, dehiscent areas in the tegmen tympani, and dehiscent suture lines of the temporal bone.
4. Spread may occur through non anatomical bony defects like those caused due to trauma, (accident, surgical) or by erosion due to neoplasia.
5. Spread may occur through surgical defects as caused by fenestration of the oval window during stapedectomy procedures.
6. Spread may occur directly into the brain tissue through the periarteriolar spaces of Virchow Robin. This spread does not affect the cortical arterioles perse, hence abscess occur in the white matter without the involvement of gray matter of brain.
Chronic middle ear disease cause complications by progressive and relentless erosion of the bone barriers, exposing the structures at risk to damage- the facial nerve, labyrinth and the dura. Acute infections cause early complications via the thrombophlebitis mechanism or extension through already available anatomical pathways.
Factors that determine the spread of infection:
I.Patient attributes: Patient's general condition and immunologic status play an important role in the spread of infections.
II.Bacterial attributes like the virulence of the infecting organism is also important. For example acute infections caused by Strep.pneumoniae type III, and H. Influenza type B have immense potential to spread.
III. Adequacy / Inadequacy of treatment of the middle ear condition may also play an important role.
Extradural abscess:
Is always associated with involvement of dura mater by the spreading disease, constituting pachymeningitis. This is commonly preceded by loss of bone, either through demineralisation in acute infection or erosion by cholesteatoma in chronic disease. If the cholesteatoma is non infected it may simply expose the dura without any inflammatory reaction. If cholesteatoma is infected it is associated with formation of granulation tissue over the dura. Dura is tough and resists infection. It attempts to wall off the infection, and collection of pus occur between the dura and the bone. This is known as extradural abscess and is the commonest of all intracranial complications. A middle cranial fossa extradural mass may strip the dura from bone on the inner surface of squamous temporal bone. Such an enlarging mass may cause increasing intracranial tension, causing focal neurological signs and papilloedema. Sometimes it could erode the skull from inside to the exterior causing a subperiosteal abscess i.e.the classic Pott's puffy tumor. Rarely an extradural abscess may develop medial to the arcuate eminence over the petrous apex. This irritates the Gasserian ganglion of the trigeminal nerve, and the 6thcranial nerve. This produces the classic Gradenigo's syndrome (includesfacial pain, diplopia and aural discharge). Posterior fossa extradural abscess is limited by the attachments of the dura laterally to the sigmoid sinus. Posterior extension of this abscess around the sigmoid sinus produces the perisinus abscess. This could also extend to the neck through the jugular vein.
Clinical features:
Depends on the site of the abscess, its size, duration and rate of development.In most patients the symptoms are vague, and non specific. Sometimes it could be a incidental finding during mastoid surgery. The common complaint of the patient being headache accompanied by malaise. If the abscess communicates with the middle ear the patient may have interim relief following an episode of aural discharge.
Management:
CTscan is diagnostic. Surgery must be done as early as possible.Granulation tissue over the dura should not be disturbed because it could breach the only defense and the infection could spread to the brain.
Subdural abscess (Empyema):
When spread of infection breaches the dura it exposes the subdural space to the perils of the infection. It may initially be associated with Leptomeningitis, or if the infection is contained as subdural effusions or subdural abscess. The rate of spread of the infection determines the clinical presentation. The dura is highly resistant to infection, the granulation tissue which develops on the inner side of the dura obliterates the subdural space. Initially seropurlent effusion develops in the subdural space, and eventually this becomes frankly purulent. The spread of this effusion is limited by the granulation tissue which attempts to obliterate the subdural space. The subdural pus tends to accumulate near the falx cerebri, that too particularly where it joins the tentorium cerebelli. Healing is always associated with fibrosis and obliteration of the subdural space in the area where granulation was present.
The cortical veins in the adjacent area may become involved by thrombophlebitis, this may be responsible for some of the clinical features. This may also produce multiple small abscess in the brain adjacent to the area of subdural infection. One or numerous multiloculated abscesses over the convex surface of the cerebral hemispheres may be seen. Commonly Non haemolytic streptococci have been implicated.
Clinical features:
The subdural empyema can be suspected by the presence of headache and drowsiness. Focal neurological symptoms like irritative fits and paralysis may follow. Fits are usually of Jacksonian type, starting locally and spreading to affect one side of the body this is usually caused by cortical thrombophlebitis. Paralysis may start with one upper or lower limb and may gradually become hemiplegia. If dominant lobe is involved aphasia develops. The site of fits and the pattern of localising signs suggests the area of empyema. Papilloedema is highly uncommon, and similarly palsies involving individual cranial nerves are also rare. Meningism may accompany headache, despite this feature this can be distinguished from meningitis by the presence of characteristic neurological localising signs. In children suspected of meningitis, subdural empyema should be considered if there is no response to treatment, or if motor seizures occur. CT scan is diagnostic. While CSF pressure may be elevated, the sugar contents are normal and the cultures are invariably sterile. In places where CT scan facilities are unavailable exploratory burr holes may be made to clinch the diagnosis.
Management:
Must be done in close coordination with neurosurgeon. Massive doses of antibiotics (systemic) like penicillin and chloramphenicol must be given. The subdural abscess must be drained and the subdural space irrigated. Ear disease must be surgically treated only after the subdural empyema has been cleared or resolved. Acute ear infections maybe treated with myringotomy and chronic infections can be managed with mastoidectomy. Neurosurgical management includes burr holing the skull thereby draining the abscess. Antiseizure drugs must be prescribed to supress seizures.
Lateral sinusthrombosis:
Thrombophlebitis can develop in any of the veins adjacent to the middle ear cavity. Of these the lateral sinus, which comprise of the sigmoid and transverse sinuses is the largest and most commonly affected. Initially it is usually preceded by the development of an extradural perisinus abscess. The mural thrombus partly fills the sinus. The clot progressively expands and eventually occlude the lumen.The clot may later become organised, and partly broken down and may even be softened by suppuration. During this stage there is a release of infecting organism and infected material into the circulation causing bacteremia, septicemia and septic embolisation.
Extension / propagation of the thrombus upwards may extend to the confluence of the sinuses, and beyond that to the superior sagittal sinus. Invasion of the superior and inferior petrosal sinuses may cause the infection to spread to the cavernous sinus. This spread of venous thrombophlebitis into the brain substance accounts for the very high association of this complication with brain abscess.Downward progression of thrombus into and through the internal jugular vein can reach the subclavian vein.
The harmful effects are caused by the release of infective emboli into the circulation, and also from the haemodynamic disturbances caused to venous drainage from inside the cranial cavity. The use of antibiotics have greatly reduced the incidence of lateral sinus thrombosis these days.
Formerly it was commonly associated with acute otitis media in childhood; now it is commonly seen in patients with chronic ear disease. In the preantibiotic era the commonest infecting organism was beta hemolytic streptococci. This organism was known to cause extensive destruction of red blood cells causing anaemia. Now a days the infection is by a mixed flora.
Clinical features:
These patients manifest with severe fever, wasting illness in association with middle ear infection. The fever is high and swinging in nature,when charted it gives an appearance of 'Picket fence'. It is always associated with rigors. The temperature rose rapidly from 39 - 40degree Centigrade. Headache is a common phenomenon, associated with neck pain. The patient appear emaciated and anaemic. When the clot extended down the internal jugular vein, it will be accompanied by perivenous inflammation, with tenderness along the course of the vein.This tenderness descended down the neck along with the clot, and would be accompanied by perivenous oedema or even suppuration of the jugular lymph nodes. Perivenous inflammation around jugular foramen can cause paralysis of the lower three cranial nerves. Raised intracranial pressure produce papilloedema and visual loss. Hydrocephalus could bean added complication if the larger or the only lateral sinus is occluded by the thrombus, or if the clot reaches the superior sagittal sinus. Extension to the cavernous sinus can occur via the superior petrosal sinus, and may cause chemosis and proptosis of one eye. If circular sinus is involved it could spread to the other eye. The propagation of the infected emboli may cause infiltrates in the lung fields, and may also spread to joints and other subcutaneous tissues..These distant effects usually developed very late in the disease, these could be the presenting features if the disease is insiduous in onset.Masking by antibiotics could be one of the causes. Patients always feel ill, and persisting fever is usual. The patients may have ear ache, in association with mastoid tenderness, and stiffness along the sternomastoid muscle. The presence of anaemia is rare now a days. Papilloedema is still a common finding. Other coexisting intracranial complications must be expected in more than 50 percent of patients. Extension of infected clot along the internal jugular vein is always accompanied by tenderness and oedema along the course of the vein in the neck, and localised oedema over the thrombosed internal jugular vein may still be seen. One rare finding is the presence of pitting oedema over the occipital region, well behind the mastoid process, caused by clotting within a large mastoid emissary vein, this sign is known as the Griesinger's sign. In fact there is no single pathognomonic sign for lateral sinus thrombosis and a high index of suspicion is a must in diagnosing this condition.
Investigations:
A lumbar puncture must be performed, if papilloedema does not suggest that raised intracranial pressure may precipitate coning. Examination of CSF is the most efficient way of identifying meningitis. In uncomplicated lateral sinus thrombosis the white blood count in the CSF will be low when the cause is chronic middle ear disease, and some what raised in acute otitis media. The CSF pressure is usually normal. The variations in the level of CSF proteins and sugar are not useful.
Queckenstedt test:
This is also known as Tobey - Ayer test. This is recommended whenever lumbar puncture for a possible intracranial infection is performed. The test involves measurement of the CSF pressure and observing its changes on compression of one or both internal jugular veins by fingers on the neck. In normal humans compression of each internal jugular vein in turn is followed by an increase in CSF pressure, of about 50 - 100mm above the normal level. When the pressure over the internal jugular vein is released then there is a fall in the CSF pressure of the same magnitude. In patients with lateral sinus thrombosis pressure over the vein draining the occluded sinus cause either no increase, or a low slow rise in CSF pressure of 10 - 20 mm.Compression of the normal internal jugular vein produces a rapid pressure rise ranging from 2 - 3 times the normal level. This test is also prone for false negative results due to the presence of collateral channels draining the venous sinuses. False positives can occur if a normal lateral sinus is small or absent that creating an erroneous impression of lateral sinus thrombosis.
CT scanning:
is an essential investigation in these patients. It may show filling defects within the sinus, and increased density of fresh clots.When contrast materials like Iothalamate (conray) is used failure of opacification of the affected lateral sinus may become evident. The presence of septic thrombosis shows intense inflammatory enhancement ofthe sinus walls and of the adjacent dura. This enhancement of the walls, but not of the contents of the sinus constitutes the empty triangle or 'delta' sign. It can also exclude accompanying complications like brain abscess and subdural empyema.
Angiography:
is a definitive investigation of lateral sinus thrombosis. It helps to demonstrate the obstruction, its site and the anatomical arrangement of the veins. There is an impending risk of displacing the infected thrombus.
Arteriography:
performed with radio opaque dye injected into the carotid artery can show the venous outflow during the venous phase. This can be clearly visualised in digital subtraction angiography. This technique involves precise superimposition of a negative arteriogram on a positive film of bone structures. This effectively cancels out the skeletal image thus clearly revealing the vascular pattern.
MRI:
Is sufficiently diagnostic hence angiography can be avoided if MRI could be taken. Established thrombus shows increased signal intensity in both T1 and T2 weighted images. MRI can also be used to show venous flow. Gadolinum enhancement may show a delta sign comparable with that seen on CT scans.
Management:
Treatment involves administration of antibiotics, together with exposure of lateral sinus and incision of the sinus and removal of its contents. Anticoagulants are not advocated at present. Before exposing the lateral sinus and clearing its contents it is imperative to clear the ear of any infections by doing a cortical mastoidectomy. The involved sinus may feel firm, appear white and opaque thus suggesting occlusion of the lumen with clot. Dissemination of clot can be prevented by ligation of the affected internal jugular vein. Now a days the only indication of internal jugular vein ligation is the presence of septicemia which is resistant to antibiotics.
Meningitis:
It is also known as Leptomeningitis.(only the piamater and arachnoid are involved). This is a major and serious complication of middle ear infection. In the pre antibiotic era the sufferers invariably died.Nowadays, recovery is usual provided early diagnosis and prompt treatment is initiated.. In pre antibiotic era meningitis was a common complication of acute middle ear infections, but now it is a frequent complication of chronic middle ear disease. Childhood otogenic meningitis is commonly caused by acute middle ear infections, in adults it is commonly a complication of chronic middle ear disease. Spread to the meninges may occur via any of the dehicences in the bony barrier or preformed channels. The rate of development depends on the virulence of the organism and the resistance of the host.
Suppurative labyrinthitis can cause meningitis via access to the cerebrospinal spaces through internal auditory meatus, and through vestibular and cochlear aqueducts. Rarely rupture of brain abscess into the subarachnoid space may lead on to meningitis. Meningitis can develop within hours of the onset of acute otitis media. The organisms usually responsible to acute infection are H. Influenza type B, and Strep.pneumoniae type III. Infections from chronic ear diseases nay be caused by gram negative enteric organisms, proteus, and psuedomonas. Anaerobes and bacteriodes have also been reported.
The initial inflammatory response of the pia arachnoid to infection is an outpouring of fluid into the subarachnoid space, with a rise in CSF pressure. The CSF becomes permeated with white blood cells and rapidly multiplying bacteria. These bacteria feed on glucose present in the CSF reducing its level in CSF a characteristic finding in meningitis. Pus initially accumulates in the basal cisterns, and more rarely in the vertex. The free flow of CSF is impeded by the exudate obstructing the ventricular foramina to cause a non communicating hydrocephalus.Obstruction to CSF in the subarachnoid spaces may cause communicating hydrocephalus. Irritation of the upper cervical nerve roots by the exudate cause neck pain and neck stiffness which are the characteristic features of this condition. Exudates around the exit foramina ofcranial nerves could cause nerve palsies during the late stage of the disease. Spread of infection through virchow robin spaces into thebrain substance may lead to the formation of brain abscess.
Clinical features:
The most reliable clinical feature of this condition is the presence of headache and neck stiffness. At first the headache could be localised to the side of the affected ear but later it could become generalised and bursting in nature. There is also associated malaise and pyrexia.Initially neck stiffness shows resistance only to flexion, but later full rigidity or retraction may develop. During early stages the patient may have mental hyperactivity and restlessness. Tendon reflexes becomes exaggerated during this stage. Photophobia is another constant presenting feature, and the patient may be prompted to lie curled up away from the light. Vomiting projectile in nature is another important feature. As the condition worsens the symptoms also become progressively severe. When neck stiffness is marked the patient may manifest positive kernigs sign. The stiffness may become more severe enough to cause opisthotonus.
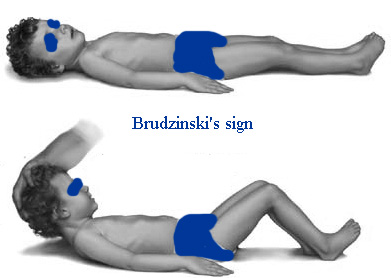
Brudzinski's sign:
Brudzinski's sign is involuntary lifting of the legs in meningeal irritation when lifting a patient's head. Kernig's sign is resistance and pain when knee is extended with hips fully flexed. Patients may also show opisthotonus; spasm of the whole body that leads to legs and head being bent back and body bowed forward.
Diagnosis:
Is made by the examination of CSF. Any patient with suspected menigitis must undergo lumbar puncture. The CSF analysis show increased white cells and reduced glucose levels from 1.7-3 mmol/l to 0.. Chloride content may fall from 120 mmol/l to 80mmol/l. Bacteria may also be isolated from the CSF. Recently polymerase chain reaction have been used to detect bacterial DNA from CSF.
Management:
The mainstay in the medical management is large doses of systemicantibiotics. Penicillin is the drug of choice. Streptomycin may also beused as an adjunct. Chloramphenicol may also be used. Ceftrioxine athird generation cephalosporin is widely used these days in thetreatment of meningitis. This has a broad spectrum activity.Metronidazole is also used because of its usefulness in treatinganaerobes. After the patient recoversfrom the acute problem, effort must be made to remove the middle earpathology which was the cause for this problem. In chronic middle earinfections modified radical mastoidectomy is the procedure of choice,in acute middle ear infections cortical mastoidectomy is the preferredsurgical procedure.
Brain abscess:
Otogenic brain abscess always develop in the temporal lobe or the cerebellum ofthe same side of the infected ear. Temporal lobe abscess is twice ascommon as cerebellar abscess. In children nearly 25% of brain abscessesare otogenic in nature, whereas in adults who are more prone to chronicear infections the percentage rises to 50%. The routes of spread ofinfection has already been discussed above, the commonest being thedirect extension through the eroded tegment plate. Although dura ishighly resistant to infection, local pachymeningitis may be followed bythrombophlebitis penetrating the cerebral cortex, sometimes theinfection could extent via the Virchow - Robin spaces in to thecerebral white matter. Cerebellar abscess is usually preceded bythrombosis of lateral sinus. Abscess in the cerebellum may involve thelateral lobe of the cerebellum, and it may be adherent to the lateralsinus or to a patch of dura underneath the Trautmann's triangle.
Stages of formation of brain abscess:
Stage of cerebral oedema: This is infact the first stage of brain abscessformation. It starts with an area of cerebral oedema and encephalitis.This oedema increases in size with spreading encephalitis. Walling off of infection by formation of capsule: Brain attempts to wall off the infected area with the formation of fibrous capsule. This formation of fibrous tissue is dependent on microglial and blood vessel mesodermal response to the inflammatory process. This stage is highly variable. Normally it takes 2 to 3 weeks for this process to be completed.
Liquefaction necrosis:Infected brain within the capsule undergoes liquefactive necrosis with eventual formation of pus. Accumulation of pus cause enlargement of the abscess.
Stage of rupture:
Enlargement of the abscess eventually leads to rupture of the capsule containing the abscess and this material finds its way into the cerebrospinal fluid as shown in the above diagram. Cerebellar abscess which occupy the posterior fossa cause raised intra cranial tension earlier than those above the tentorium. This rapidly raising intra cranial pressure cause coning or impaction of the flocculus or brain stem into the foramen magnum. Coning produces impending death. If the walling off process (development of capsule) is slow, softening of brain around the developing abscess may allow spread of infection into relatively avascular white matter, leading to the formation of secondary abscesses separate from the original or connected to the original by a common stalk. This is how multilocular abscesses are formed. Eventually the abscess may rupture into the ventricular system or subarachnoid space, causing meningitis and death.
The mortality rate of brain abscess is around 40%, early diagnosis after the advent of CT scan has improved the prognosis of this disease considerably..
The bacteriological flora is usually a mixture of aerobes and obligate anaerobes. Anaerobic streptococci are the commonest organisms involved. Pyogenic staphylococci is common in children. Gram negative organim like proteus, E coli and Pseudomonas have also been isolated.
Clinical features:
The earliest stage where the brain tissue is invaded (stage of encephalitis) is marked by the presence of headache, fever, malaise and vomiting. Drowsiness eventually follow. These early features may be masked by the complications such as meningitis or lateral sinus thrombosis. If this stage progresses rapidly to generalised encephalitis before it could be contained by the formation of the capsule, drowsiness may progress to stupor and coma followed by death..Usually the period of local encephalitis is followed by a latent period during which the pus becomes contained within the developing fibrous capsule. During this latent phase the patient may be asymptomatic.
During the next state (stage of expansion) the enlarging abscess first cause clinical features due to the alteration of CSF dynamics, and site specific features may also be seen due to focal neurological impairment. The pulse rate slows with rising intracranial pressure,the temperature may fall to subnormal levels. Drowsiness may alternate with periods of irritability. Papilloedema is also found due to elevated CSF pressure.
Clinical features also vary according to the site of involvement. Hence thedifferences that are seen between the cerebral and cerebellar abscess.
Cerebral (Temporo sphenoidal abscess):
A cerebral abscess in the dominant hemisphere often cause nominal aphasia, where in the patient has difficulty in naming the objects which are in day to day use. He clearly knows the function of these objects. Visual field defects arise from the involvement of optic radiations. Commonly there is quadrantic homonymous hemianopia,affecting the upper part of the temporal visual fields, more rarely it may also involve the lower quadrants. The visual field loss are on the side opposite to that of the lesion. This can be assessed by confrontation method. Upward development affects facial movements on the opposite side, and then progressively paralysis of the upper and lower limbs. If the expansion occur in inward direction then paralysis first affects the leg, then arm and finally the face.
Cerebellar abscess:
The focal features associated with cerebellar abscess is weakness and muscle incoordination on the same side of the lesion. Ataxia causes the patient to fall towards the side of the lesion. Patient may also manifest intention tremors which may become manifest by the finger nose test. This test is performed by asking the patient to touch the tip of the nose with the index finger first with the eyes open and then with the eyes closed. The patient may often overshoot the mark when attempted with the eyes closed in case of cerebellar abscess. The patient may also have spontaneous nystagmus. Dysdiadokinesis is also positive in these patients.
Investigations:
CT scan and MRI scans are the present modes of investigation. Scan is ideally performed using contrast media. These scans not only reveal the position and size of the abscess, the presence of localised encephalitis can be distinguished from that of an encapsulated abscess.Associated conditions such as subdural abscess, and lateral sinus thrombosis can also be seen.
Lumbar puncture: Isfrought with danger because of the risk of coning. Lumbar puncture mustbe performed in these patients only in a neurosurgical unit whereimmediate intervention is possible if coning occurs.
Treatment:
involves use of large doses of antibiotics. Ideally the abscess shouldbe controlled neurosurgically and with antibiotics. After the patientrecovers mastoidectomy is performed to remove the focus of infection.Abscess can be drained by placement of burr holes, and excision of thenecrotic tissue along with the capsule.
Otitic hydrocephalus:
Is one of the common complication of middle ear infection. It is a syndrome of raised intracranial pressure during or following middle ear infection. This condition is also known as Pseudotumor cerebri.
Pathogenesis:
The aetiology is unknown. The relationship of this condition with that oflateral sinus thrombosis has been documented. The inference is thatobstruction of the lateral sinus affects cerebral venous outflow, orthe extension of the thrombus into the superior sagittal sinus impedesCSF resorption by pacchionian bodies.
Clinical features:
The leading symptoms are
1. headache
2. drowsiness
3. blurred vision
4. nausea
5. vomiting
6. diplopia (rarely)
The onset may occur many weeks after acute otitis media, or many yearsafter the start of the chronic middle ear disease. Clincial examinationmay show papilloedema. Lateral rectus palsy on one or both sides arealso commonly seen. This occur due to the stretching of the 6th nervedue to increased intracranial pressure. CT scan is diagnostic.
Treatment:
Revolves around the management of the elevated intra cranial tension. It includes use of steroids, diuretics and hyperosmolar dehydrating agents. Repeated lumbar punctures may also be used to reduce the tension. Surgical clearance of the infection of the middle ear should also follow.