Autophony current trends in management
Contents
Definition:
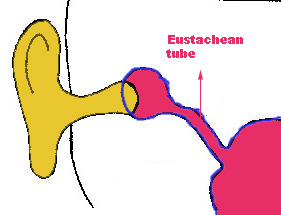
Autophony literally means hearing one's voice in one's own ear. This condition is commonly caused by a persistently open eustachean tube.
Pathophysiology:
In Autophony air flows into the middle ear cavity from the nasopharynx on a continuing basis through a persistantly open eustachean tube causing a roaring noise when ever the patient takes a breath. These patients irked by hearing their own voice in the ear, starts to speak in a whisper. These patients become so upset psychologically, they turn recluse and become depressed.
The exact mechanism causing autophony still remains unknown. CT scan in these patients show atrophy of soft tissues surrounding the tube. The possibility of this atrophy keeping the eustachean tube open should be considered.
Peculiar features of autophony is that it gets releived when the patient lies on his back or when bending at the waist. These two manouvers close the eustachean tube. These patients also have a peculiar habit of sniffing frequently in an attempt to close the pharyngeal end of eustachean tube.
Etiology:
Possible etiological factors causing autophony include:
1. Weight loss
2. Autoimmune disorders like Wegener's granuloma, Bell's palsy, Crohn's disease, Meniere's disease.
How these autoimmune conditions cause autophony is still not clear. About 1/3 of patients with autophony have autoimmune disorder.
Females are commonly affected than males. Unilateral autophony is common than bilateral involvement.
Investigations:
1. Impedance auditometry
2. Sonotubometry
Treatment:
The aim of treatment is directed towards reducing the size of the eustachean tube. It is hence possible to reduce the size of eustachean tube by inserting silicone tubing of 1mm size through the middle ear end of eustachean tube past the isthumus.
If the eustachean tube opening is very large then silicone block can be inserted via the middle ear end of eustachean tube. After this procedure it is better to insert a ventilation tube to prevent fluid accumulation in the middle ear cavity.
Microdebrider eustachean tuboplasty:
Before performing tuboplasty, CT scan of paranasal sinuses must be done. If there is evidence of sinusitis then FESS surgery should be combined with tuboplasty. It is always better to perform tuboplasty before sinus surgery to ensure dry field.
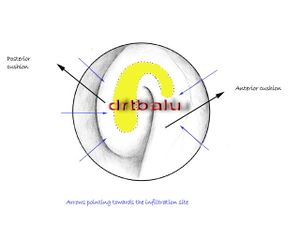
The whole surgical procedure can be performed under local anesthesia. Topical anesthesia is provided by placing cotton pledgets dipped in 4% xylocaine with 1 in 10,000 units adrenaline. Infiltrative anesthesia is provided by injecting 1% xylocaine with 1 in 10,0000 units adrenaline. This solution is injected along the entire posterior eustachean tube cushion. Injections are also given along the superior portion of the anterior cushion.
Microdebrider is used to remove excessive soft tissue from the posterior eustachean tube cushion. Tissure removal is started in the midportion of the posterior cushion. Injury to the mucosa over the anterior cushion should be avoided, as it could cause scarring. The cutting surface of the debrider should always be directed towards the posterior cushion. Debriding is continued till the valvular area is reached i.e. the junction between the anterior and posterior cushions.
- Caution: All soft tissue removal should be superficial to the tubal cartilage to prevent damage to the carotid artery. *
Lasers can be used to perform Eustachean tuboplasty.