Applied anatomy of recurrent laryngeal nerve
Introduction:
In order to understand the various neurological problems affecting the mobility of the vocal cord a clear understanding of the anatomy of recurrent laryngeal nerve is a must because it supplies the muscles acting on the vocal cord. The larynx is intimately involved in swallowing, breathing, coughing and phonation. These functions are dependent on normal movements of the vocal cords. These movements are controlled by muscles which are innervated by the recurrent laryngeal branch of the vagus nerve. The traditional textbooks of otolaryngology divided the etiology of recurrent laryngeal nerve paralysis by applying the rule of one thirds.
The rule of one third states that recurrent laryngeal nerve palsy is caused by tumors in 1/3 of cases, trauma in 1/3 of cases and causes unknown in 1/3 of the cases (idiopathic). New surgical procedures, along with the evolution of better investigation techniques have reduced the idiopathic causes of recurrent laryngeal nerve palsy.
Anatomy:
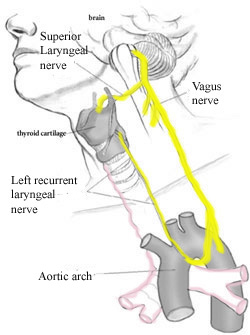
The recurrent laryngeal nerve is a myelinated nerve. It is a component of the vagus nerve. As the vagus nerve exits the medulla, the fibers of the recurrent laryngeal nerve are anteriorly situated in it. As the vagus traverses inferiorly, the fibers of the recurrent laryngeal nerve starts to rotate medially until they are ultimately separated from the vagus nerve. The vagus nerve has a superior ganglion at the level of the jugular foramen.. This ganglion is also known as jugular ganglion. This ganglion contains cell bodies of parasympathetic and sensory fibres that run in the vagus.
Inside the jugular foramen the vagus nerve consists of multiple bundles of nerve fibers. Tumors in the jugular foramen can infiltrate these fasicles without loss of vagal integrity. The vagus nerve leaves the skull base via the jugular foramen anterior to the jugular vein. The vagus then assumes a more posterior position medial to the jugular vein. The vagus nerve has an inferior ganglion also known as the nodose ganglion immediatly below the jugular foramen. The vagal supply to the pharyngeal plexus and the superior laryngeal nerve arise from this ganglion.
The course taken by the vagus nerve differs between the right and the left sides. The left vagus nerve follows the carotid artery into the mediastinum crossing anterior to the aortic arch. The recurrent laryngeal nerve arising from the vagal nerve just below the aortic arch loops medially under the aorta and ascends within the tracheoesophageal groove. The anterior bronchoesophageal artery supplies the left vagus nerve. The right vagus nerve descends with the common carotid artery. At the level of division of the innominate artery, the right recurrent laryngeal nerve loops around the subclavian artery and ascends along the superior lobe of the pleura. It then approaches the trachoesophageal groove behind the common carotid artery. The approximate length of the left recurrent laryangeal nerve is 12 cms, where as the right nerve measures about 6 cms only. Considering the extra length and the distance the left recurrent laryngeal nerve has to travel, it is the common nerve affected by diseases / disorders / trauma etc. The right recurrent laryngeal nerve does not get into the tracheoesophageal groove until it approaches the cricothyroid joint. In some patients the right recurrent laryngeal nerve is given off from the vagus nerve at the level of thyroid gland, this condition is always associated with an anomalous retroesophageal location of the right subclavian artery. This is also known as a non recurrent variation of the right recurrent laryngeal nerve. This condition palces the nerve at risk during thyroid surgery.
Relationship of recurrent laryngeal nerve with inferior thyroid artery: The recurrent laryngeal nerve has significant but varying relationship with the inferior thryoid artery. On the left side, the recurrent laryngeal nerve passes behind the inferior thyroid artery in 50% of the cases and anterior to the artery in 20% of cases and may lie in between the branches of the inferior thyroid artery in 30% of cases. On the right side since the recurrent laryngeal nerve approaches the traceoesophageal groove more laterally, these relations are different on the right side. In half of the cases the recurrent laryngeal nerve passes between the distal branches of the inferior thyroid artery, in 30% of patients it may lie anterior to the artery, and in 20% of cases it may lie deep to the inferior thyroid artery.
The recurrent laryngeal nerve enters the larynx deep to the inferior constrictor muscle and posterior to the cricoarytenoid joint. Inside the larynx it divides into a sensory and motor branches. The anteriorly directed motor branch is made up of 1000 axons. About 250 of the axons innervate the cricoarytenoid muscle, since it is the sole abductor of the vocal fold. The trachea, oesophagus and pyriform sinuses receive their sensory fibers from the posterior division of the recurrent laryngeal nerve before entering the larynx.
The blood supply to the recurrent laryngeal nerve comes from the inferior thyroid artery. The feeding branches are usually anterior to the nerve. Distally, the inferior laryngeal artery, a terminal branch of the inferior thyroid artery, supply the recurrent laryngeal nerve
Etiology of damage to recurrent laryngeal nerve:
The left recurrent laryngeal nerve is more susceptible to injuries than the right because of its longer and more extensive course. It also lies superficial in the left tracheoesophageal groove. The recurrent laryngeal nerve can be damaged by vascular insults, viral infections, bacterial infections (tuberculosis affecting the apex of the right lung cause involvement of right recurrent laryngeal nerve because of its proximity to the right apex), neurotoxic drugs, tumors and trauma have all been implicated The recurrent laryngeal nerve is at risk during surgeries involving the neck, chest, skull base. The potential for recovery is generally proportional to the degree of injury. Slow growing tumors that engulf and infiltrate the nerve generally allow compensation for paralysis.