Chronic Suppurative Otitis Media
Contents
- 1 Definition:
- 2 Types of chronic suppurative otitis media:
- 3 Tubotympanic disease:
- 4 Microbiology of CSOM:
- 5 Clinical features of tubotympanic disease:
- 6 Pathology of tubotympanic disease:
- 7 Management of tubotympanic disease:
- 8 Atticoantral type of disease (Unsafe type of disease):
- 9 Theories of bone invasion by cholesteatoma:
- 10 Types of cholesteatoma:
- 11 Theories to explain pathogenesis of cholesteatoma:
- 12 Clinical features of acquired cholesteatoma:
- 13 Management:
Definition:
Chronic suppurative otitis media is defined as a chronic infection of the mucosa lining the middle ear cleft. Middle ear cleft include the eustachean tube, hypotympanum, mesotympanum, epitympanum, aditus and mastoid air cell system.
Types of chronic suppurative otitis media:
Chronic suppurative otitis media is of two types:
1. Tubotympanic disease (safe type)
2. Atticoantral disease (unsafe type)
Tubotympanic disease:
This is also known as safe disease because it is bereft of any serious complications. The infection is limited to the mucosa and the antero inferior part of the middle ear cleft, hence the name. This disease does not have any risk of bone erosion. The discharge any will flow through a perforation present in the pars tensa portion of the ear drum. This perforation is usually surrounded by a rim of remnant ear drum or at least the annulus is intact. (Central perforation). The perforation is usually reniform (kidney shaped) because of poor blood supply to the affected portion of the tympanic membrane.
The infective activity of safe disease is related to the frequency of upper respiratory tract infections, the discharge tending to increase with increasing frequency of upper respiratory infections.
Aetiology:
1. Could be a sequelae to inadequately treated acute otitis media.
2. Acute suppurative otitis media causing persistant perforation which could be infected from bacteria in the external auditory canal. This condition is knonw as persistant perforation syndrome.
Microbiology of CSOM:
In all varieties of CSOM the major organism found in the discharge are gram negative bacilli i.e. Ps. aeruginosa, E. coli, and B. proteus. These organisms are not commonly found in the upper respiratory tract, but they are found in the skin of external auditory canal.
Clinical features of tubotympanic disease:
1. The discharge in this condition is profuse and mucopurulent in nature.
2. The discharge is not foul smelling.
3. Since the infected area is open at both ends i.e. the eustachean tube end and the perforation in the ear drum, the discharge does not accumulate in the middle ear.
4. The ossicular chain is not at risk in this type of disorder, the conductive deafness caused is due to the presence of perforation in the tympanic membrane and thickening of the tympanic membrane.
5. Conductive deafness may also be accentuated by thickening of round window membrane due to the presence of secretions. Hearing loss is usually about 30 - 40 dB.
6. These patients have poorly pneumatised / sclerosed mastoid air cell system. This feature has been attributed to repeated attacks of middle ear infections during childhood causing inadequate pneumatisation of mastoid air cell system. In patients with pneumatised mastoid air cell system repeated middle ear infections can cause sclerosis with evidence of new bone formation. Mastoids in these patients may be sclerotic.
7. Pain in the ear when present is always associated with otitis externa. This commonly occurs when the patient attempts to clean the ear off the purulent secretions with a ear bud or cotton tipped applicator.
Pathology of tubotympanic disease:
Pathological changes depend on the stage of the disease. The stages are as follows:
Acute stage:
This is where the ear is actively discharging. The mucosa of the middle ear cavity is hypertrophied, and congested.
Inactive stage:
This condition is characterised by dry perforation of ear drum, commonly in its antero inferior part, close to the eustachean tube orifice. The middle ear mucosa is normal.
Quiescent stage:
Perforation of ear drum is present, the middle ear is dry and mucosa may be normal or hypertrophied.
Healed stage:
Here the perforation of ear drum has healed by formation of thin scar. There may even be tympanosclerotic patches / chalky deposits on the ear drum. The ossicular chain is invariably intact.
Tuning fork tests show:
Rinne - Negative on the affected side
Weber - Lateralised to the good ear
Absolute bone conduction test - Not reduced
Pure Tone audiometry show conductive hearing loss. The hearing loss is invariably under 40 dB.
Management of tubotympanic disease:
Conservative management:
If the disease is active - with active ear discharge
Aural toileting - must be done using dry cotton swabs.
Suction method can be used to suck out secretions from the external canal and the middle ear cavity. The only disadvantage of this procedure is the risk of noise induced deafness.
Syringing the affected ear with warm saline mixed with acetic acid (1.5%) can be used to syringe the affected ear. This solution not only clears the ear of its purulent secretions, it also helps to remove crusts if present. The presence of weak acetic acid has bacteriostatic effect.
Role of antibiotics in the management of tubotympanic disease:
Antibiotics can be administered depending on the culture report. The best route of administration is topical because the presence of a large central perforation enables adequate concentration of antibiotics to reach the middle ear mucosa. Ototoxic drugs are to be avoided because the increased vascularity present in the middle ear mucosa will cause easy absorption of the drug into the inner ear fluids causing sensori neural hearing loss. Ciprofloxacillin can be administered topically.
Oral amoxycillin in adequate doses or penicillins in adequate doses may be beneficial.
Role of antihistamines and nasal decongestants: Is questionable. Their role is to decongest the nasal and naso pharyngeal mucosa, pharyngeal end of eustachean tube. Since there is associated perforation of tympanic membrane, secretions dont tend to accumulate inside the middle ear cavity. Topical nasal decongestants should not be used for more than a week, because of their propensity to cause rhinitis medicamentosa.
Precautions:
1. The ear must be kept dry. This can be achieved by keeping the ears plugged when taking head bath. Swimming must be avoided till the perforation heals.
2. Pre existing sinus infections if any must be treated aggressively.
3. Presence of focal sepsis in the throat (tonsils commonly) must be ruled out.
Surgical management:
1. Surgical management aims at correcting the causative problems if any.
The presence of deviated nasal septum must be corrected as this could predispose to chronic sinus infections.
If focal sepsis is identified in the tonsils and adenoid then adenotonsillectomy needs to be performed.
After eradicating the possible focal sepsis only attempt must be made to definitively treat the perforation. If the ear drum has managed to stay dry for more than 6 months myringoplasty can be performed. Temporalis fascia is used as grafting material because of its availability in close proximity, its thickness is more or less similar to that of normal ear drum. One other added advantage is its low basal metabolic rate.
If middle ear mucosa is wet and oedmatous then cortical mastoidectomy should be resorted to if conservative management fails. Mastoidectomy can always be combined with myringoplasty in the same sitting.
Atticoantral type of disease (Unsafe type of disease):
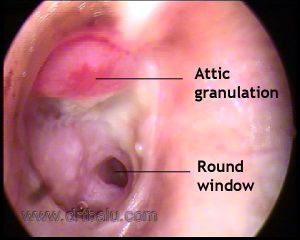
This is termed as unsafe because dangerous intra cranial and extra cranial complications can occur, proving fatal to the patient. This disease spreads by erosion of the bony wall of the attic. Cholesteatoma is commonly present in this condition. This disease is commonly seen in sclerosed mastoid cavities. Presence of granulation tissue is also common in this disorder.
This condition mainly affects the attic region of the middle ear. This region is pretty crowded, with the presence of the head of the malleus and incus. Any disease process involving crowded portions tend to cause more complications. Bone erosion occurs due to the presence of osteitic reaction in the bone tissue.
Definition of cholesteatoma: Cholesteatoma is defined as a cystic bag like structure lined by stratified squamous epithelium on a fibrous matrix. This sac contains desquamated squamous epithelium. This sac is present in the attic region. Cholesteatoma is also defined as 'skin in wrong place'. Cholesteatoma is known to contain all the layers of skin epithelium. The basal layer (germinating layer) is present on the outer surface of cholesteatoma sac in contact with the walls of the middle ear cleft.
Theories of bone invasion by cholesteatoma:
1. Pressure theory - states that increase in the pressure caused by enlarging cholesteatoma cause bone erosion. Ischemia has been attributed as the cause in this theory.
2. Enzymatic theory: Inside the cholesteatoma are present multinucleated osteoclasts and histiocytes. These cells release acid phosphatase, collagenase and other proteolytic enzymes. These enzymes are known to cause bone erosion.
3. Pyogenic osteitis: Pyogneic bacteria may release enzymes which could cause bone resorption.
Types of cholesteatoma:
1. Congenital cholesteatoma
2. Primary acquired cholesteatoma
3. Secondary acquired cholesteatoma
Congenital cholesteatoma:
is known to arise from embryonic cell rests present in the middle ear cavity and temporal bone. These cell rests are known to commonly occur in cerebello pontine angle and petrous apex. Infact congenital cholesteatoma is seen as a whitish mass behind an intact tympanic membrane.
Derlacki and Clemis laid down the following as criteria to diagnose congenital cholesteatoma:
1. The patient should not have previous episodes of middle ear disease
2. Ear drum must be intact and normal
3. It is purely an incidental finding
4. If discharge and ear drum perforation is present then it should be construed that congential cholesteatoma has managed to erode the tympanic membrane.
Clinical features:
The disorder is an incidental finding. The common location of congenital cholesteatoma is the antero superior quadrant of tympanic membrane, postero superior quadrant being the next common site of involvement. Anteriorly situated congenital cholesteatomas are known to affect the eustachean tube function causing conductive deafness due to middle ear effusion, where as posterior congenital cholesteatoma is known to cause conductive deafness due to impairment of ossicular chain mobility.
Staging of congenital cholesteatoma:
Staging as suggested by Derlacki and Clemis: They were the first to stage congenital cholesteatoma. They classified congenital cholesteatoma into
1. Petrous pyramid cholesteatoma
2. Cholesteatoma involving the mastoid cavity
3. Cholesteatoma involving the middle ear cavity.
Potsic suggested the following staging mechanism:
Stage I : Single quadrant involvement with no ossicular / mastoid involvement.
Stage II : Multiple quadrant involvement with no ossicular / mastoid involvement
Stage III : Ossicular involvement without mastoid involvement
Stage IV : Mastoid extension
Nelson's staging:
Type I : Involvement of mesotympanum without involvement of incus / stapes
Type II : Involvement of mesotympanum / attic along with erosion of ossicles without extension into the mastoid cavity
Type III : Involvement of mesotympanum with mastoid extension
Staging this disease will help in deciding the modality of treatment and in predicting the long term prognosis.
Acquired Cholesteatoma: can be divided into two types, primary acquired and secondary acquired cholesteatomas.
Primay acquired cholesteatoma: In this condition there is no history of preexisting or previous episodes of otitis media or perforation. Lesions just arise from the attic region of the middle ear.
Secondary acquired cholesteatoma: always follows active middle ear infection which manages to destroy the ear drum along with the annulus. This type of destruction is common in acute necrotising otitis media following exanthematous fevers like measles etc.
Theories to explain pathogenesis of cholesteatoma:
Various theories have been postulated to explain the pathogenesis of cholesteatoma. They are:
1. Cawthrone theory: This theory suggested by cawthrone in 1963 suggested that cholesteatoma always originated from congential embryonic cell rests present in various areas of the temporal bone.
2. Theory of immigration: This theory was suggested by Tumarkin. He was of the view that cholesteatoma was derived by immigration of squamous epithelium from the deep portion of the external auditory canal into the middle ear cleft through a marginal perforation or a total perforation of the ear drum as seen in acute necrotising otitis media.
3. Theory of invagination: This theory was suggested by Toss. He theorised that persistent negative pressure in the attic region causes invagination of pars flaccida causing a retraction pocket. This retraction pocket becomes later filled with desquamted epithelial debris which forms a nidus for the infection to occur later. Common organisms known to infect this keratin debris are Psuedomonas, E. coli, B. Proteus etc.
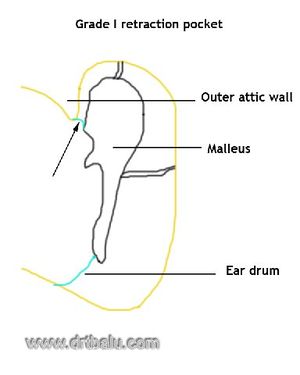
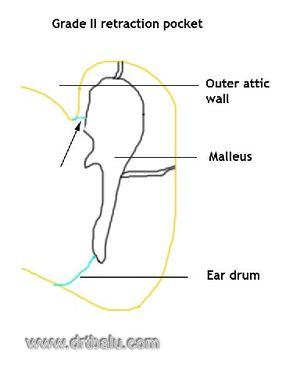
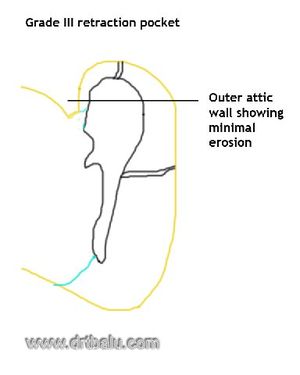
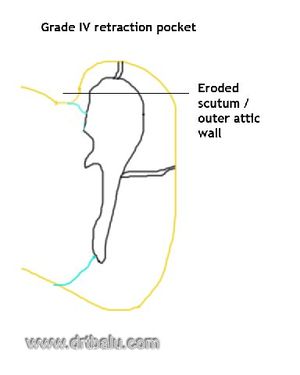
Toss also classified attic retraction pockets into 4 grades:
1. Grade I: The retracted pars flaccida is not in contact with the neck of the malleus.
2. Grade II: The retracted pars flaccida is in contact with the neck of the malleus to such an extent that it seems to clothe the neck of the malleus.
3. Grade III: Here in addition to the retracted pars flaccida being in contact with the neck of the malleus there is also a limited erosion of the outer attic wall or scutum.
4. Grade IV: In this grade in addition to all the above said changes there is severe erosion of the outer attic wall or scutum.
4. Metaplastic theory: This theory was first suggested by Wendt in 1873. He took into consideration the histological changes seen in various portions of the middle ear cavity. The attic area of the middle ear cavity is lined by pavement type of epithelium. This epithelium undergoes metaplastic changes in response to subclinical infection. This metaplastic mucosa is squamous in nature there by forming a nidus for cholesteatoma formation in the attic region.
Of all the above mentioned theories, thetheory of invagination appears to be the most plausible one currently explaining the various pathologic features of cholesteatoma.
Clinical features of acquired cholesteatoma:
Ear discharge: is scanty and foul smelling. In fact the odor is best described as musty in nature. This is due to the presence of saprophytic infection and osteitis.
Hearing loss: is commonly conductive in nature. Some patients may even surprisingly have a normal hearing despite the presence of a huge cholesteatoma. This normal hearing could be attributed to the bridging effects of cholesteatomatous mass.
Sensorineural hearing loss if present could be attributed to the absorption of toxins through the round window membrane, or may be due to use of ototoxic antibiotics topicallyon a long term basis. Ear ache: if present could be attributed to the presence of co existing otitis externa, or presence ofextradural abscess.
Tinnitus if present may indicate imminent sensorineural hearing loss. Vertigo may be present if there is erosion of lateral semicircular canal by the cholesteatomatous matrix. Fistula test if performed is positive in these patient.
Fistula test: This test is positive if there is a third window is present in the laryrinth due to the erosion of the labyrinthine bone. This commonly occurs in the lateral semicircular canal area. This test is performed using a snugly fitting siegles pneumatic speculum and slowly applying pressure by compressing the pneumatic bulb. If labyrinthine fistula is present the patient will feel giddy and will have nystagmus.
Facial palsy may indicate erosion of facial nerve canal with involvement of facial nerve.
On examiantion:
There is destruction of the outer attic wall, with presence of attic perforation. Cholesteatomatous flakes maybe seen through the perforation like cotton wool.
There is associated sagging of the posterior superior meatal wall. Hearing tests indicate conductive deafness commonly if labyrinth is uninvolved. It may turn out to be sensorineural hearing loss if there is associated erosion of the labyrinth.
X ray mastoids may show slcerosis with presence of cavity.
Management:
Since this is a surgical problem modified radical mastoidectomy is advocated in almost all of these patients. The aims of the surgical procedure is as follows:
1. To exteriorise the disease
2. To create adequate ventilation to the middle ear cavity
3. To create a permanent skin lined cavity exposed to the exterior.
The various modifications of mastoidectomy procedures are discussed elsewhere.