Evaluation of thyroid nodule
Contents
Introduction:
Nodules affecting the thyroid glands are common clinical entities. Palpation of thyroid gland put the incidence of nodule to be about 7%. Ultrasound examinations of thyroid gland put the incidence of thyroid nodule to be about 40%. This is due to the discovery of smaller nodules that would go undetected by palpation (smaller than 1.5 cms). If a nodule is identified in the thyroid gland malignancy should always be ruled out. Various investigations can be used to determine whether the detected nodule in the thyroid is benign or malignant. They are :
1. Radio isotope scans
2. Ultrasonography
3. CT / MRI scans
4. FNAC
Clinical features:
1. Nodules are mostly asymptomatic in most of the patients.
2. Malignancy should be suspected if:
a. There is history of previous neck irradiation
b. There is rapid increase in the size of the nodule
c. There are symptoms of compression like dysphagia, dysphonia, and hemoptysis
d. If the patient is a male
e. If the age of the patient is less than 20 or more than 60
f. Family history of thyroid malignancy or Multiple endocrine neoplasia.
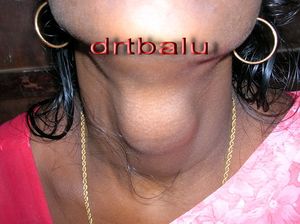
Palpation:
It is very difficult to pick out thyroid nodules less than 1.5 cm by palpation. The sensitivity of palpation varies from individual to individual. Moreover it is very difficult to palpate any nodule in a patient with thick and short neck. Nodules which are more than 4 cm are sinister. If these nodules are fixed to the skin and adjacent structures then extraglandular spread of malignancy will have to be suspected.
A palpable neck node along with a firm thyroid nodule should always lead to suspicion of thyroid malignancy with nodal metastasis.
On palpation if the thryoid nodule is irregular, tender, and firm then thyroiditis should be suspected.
On laryngeal examination if there is recurrent laryngeal nerve paralysis then malignancy should be strongly suspected.
Laboratory evaluation:
Every patient with thyroid nodule should undergo a complete hormone assay. The various hormone assays can be utmost complimentary in the diagnosis of malignancy except calcitonin. Elevated calcitonin levels are a clear cut indicator for parathyroid malignancy.
1. TSH estimation
2. T3
3. T4
4. Thyroglobulin antibody
5. ESR
6. Thyroid peroxidase antibody
7. Microsomal antibody
8. Complete blood count
9. Calcitonin
In all patients with thryoid nodule, functional status of thryoid gland will have to be ascertained. This can be done by estimating serum T3 and T4 levels. The levels of these hormones are dependent on the circulating levels of thryoglobulin. Circulating T3 and T4 hormones are bound to thyroglobulin. It is the free T3 and T4 that must be estimated. A more accurate assay would be free T4 estimation. This estimation correlates better with the functional status of thryoid gland.
TSH assay:
This is actually a highly sensitive test. This is the only test that needs to be performed to detect abnormalities of thyroid function. This test is so sensitive that it will pick up thyroid function abnormality before fluctuations in T4 can be detected. Majority of patients with thyroid nodules are euthyroid, and thus thyrotropin (TSH) levels in them will be normal. When an abnormal TSH result is obtained then the levels of T3 and T4 must compulsarily be obtained. Reduced levels of TSH may indicate hyperthyroidism (autonomic functioning gland / thyrotoxicosis), where as elevated TSH levels indicate hypothyroidism or thyroiditis. In both of these situations the thyroid gland may be enlarged or nodular.
Complete blood count and ESR: This is a must when the clinician suspects an inflammatory or infectious thyroiditis.
Thyroid peroxidase antibody assay is useful for diagnosing Hashimoto's thyroiditis. In Hashimoto's thyroiditis there is increased risk of malignancy.
Estimation of thyroglobulin:
Many conditions may cause falsely elevated or decreased levels of thyroglobulin.
Factors that cause an increase in the levels of thyroglobulin include:
1. TSH receptor stimulation
2. Volume of the thryoid gland
3. Imjury to the thryoid gland
4. Multinodular goitre
5. Smoking
6. Estrogen levels
7. Benign and malignant conditions of thyroid
This test is best used in the follow up of patients with thyroid cancer after thyroidectomies.
Radioisotope scanning:
This was one of the most important imaging modality in the diagnosis of thyroid function. But now it has fallen out of favour. The most commonly used isotopes include Technitium 99 and iodine 123. Both these isotopes provide similar information. I 123 is more physiologic than technitium 99.
Technitium 99 gets washed out of the gland and hence allows for shorter scanning time (20-30 minutes). Scanning can be immediatly started after adminsitering Technitium 99. If I123 is used then scanning can be started only after 24 hours after administration of the isotope. The scanning time lasts atleast 4 - 6 hours. Radiation exposure is more or less similar for both isotopes. Imaging resolution is better with Technitium 99 than radioiodine. Nodules below 1cm cannot be reliably detected by either of these scanning modality. Radioactive iodine scans can identify hot and cold nodules. The incidence of malignancy is more in cold nodule than hot nodule. Hot nodule is hyperfunctioning thyroid nodule, where as a cold nodule is a hypofunctioning nodule.
Indications of thyroid scan:
1. Identification of a functional solitary nodule when initial serum TSH is decreased.
2. If FNAC is reported as follicular neoplasm or suspicious lesion then the finding of Hot nodule in a scan may decrease the suspicion of malignancy
3. Detecting neck node metastatis.
Thallium - 201 scan: is a very useful diagnostic tool to differential benign and malignant thyroid nodules. Three mCi of Thallium - 201 is used to image the thyroid gland. the uptake of the isotope is categorized into low uptake, intermediate uptake and high uptake. The risks of malignancy is more in high uptake lesions, and low in low uptake lesions.
CT scan of thyroid:
CT scans are highly sensitive in detecting thyroid nodules. It is more useful to reveal mediastinal extension, retrotraheal extension and retroclavicular extension of the mass. Since the gland contains high iodine content, the brightness of the gland is increased on a CT even without contrast.
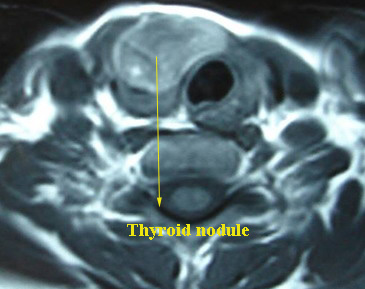
MRI scan:
It plays a minor role in the evaluation of thyroid nodule. Its major advantage over CT scan is that contrast agent (gadoliunum) can be used without causing any interference to Radio nucleotide scanning.
Ultrasound:
This is the most commonly used imaging modality for evaluating thyroid nodules. Ultrasound is commonly performed using high frequency transducers (7-13 MHz). It can detect solid nodules of 3mm to 4 mm and cystic nodules of 2mm in diameter. Cystic nodules have a lower risk of malignancy when compared to solid nodules.
Ultrasound features suggestive of malignancy include:
1. Absent Halo sign
2. Solid or hyperechogenicity
3. Heterogenous echo structure
4. Irregular margins
5. Presence of fine calcifications
6. Extraglandular extension
Fine needle aspiration cytology:
Is the gold standard in evaluation of thyroid nodule. Since a majority of thyroid nodules are benign, this test is a must to identify the rarer malignant nodule. Two types of smears are prepared. Air dried and wet smears.
Dry smear: Two methods can be used. Diff - Quick method and May Grunwald - Giemsa methods. In quick dry method, the aspirate is expelled on to a glass slide, and is air dried. This method is best for immediate reading by the pathologist. The dried smear highlights the background colloid, cell architecture and cytoplasmic details. This technique is useful in the diagnosis of medullary and lymphoid tumors.
The wet smear (papanicolaou) is a wet smear that requires immediate fixation with 95% alcohol. This method is best suited for detecting papillary cancer.
Ancillary procedures can be used to improve the accuracy of FNAC. These include:
1. Immunohistochemistry
2. Ploidy studies
3. Molecular markers
4. Reverse polymerase chain reaction
FNAC is the most important method in the diagnosis of malignant nodule.